وظائف الكلى
| أميرة ساهم بشكل رئيسي في تحرير هذا المقال
|
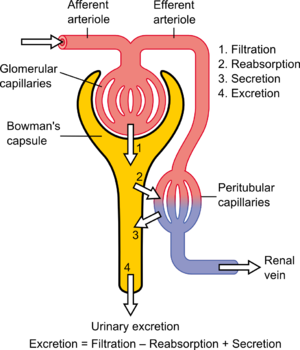
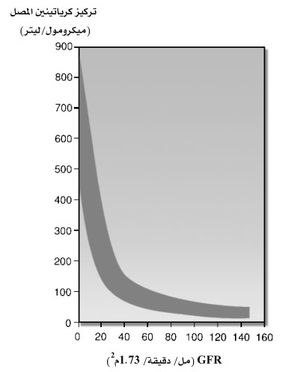
وظائف الكلى Renal function في طب الكلى, هو مؤشر على حالة الكلى ودورها في الفسيولوجيا الكلوية. معدل الرشحي الكبي (GFR) يصف معدل تدفق الساحل المرشح من خلال الكلى. معدل إزالة الكرياتينين (CCr أوCrCl) هو حجم بلازما الدم لإزالة الكرياتينين في وحدة الزمن والقياس المفيد لمعدل الرشح الكبي التقريبي.. Creatinine clearance exceeds GFR due to creatinine secretion which can be blocked by cimetidine. Alternatively, over estimation by older serum creatinine methods resulted in an under-estimation of creatinine clearance which provided a less biased estimate of GFR[1]. Both GFR and CCr may be accurately calculated by comparative measurements of substances in the blood and urine, or estimated by formulas using just a blood test result (eGFR and eCCr).
The results of these tests are important in assessing the excretory function of the kidneys. For example, grading of chronic renal insufficiency and dosage of drugs that are primarily excreted via urine are based on GFR (or creatinine clearance).
It is commonly believed to be the amount of liquid filtered out of the blood that gets processed by the kidneys. Physiologically, these quantities (volumetric blood flow and mass removal) are only related loosely.
علامات غير مباشرة
معظم الأطباء يستخدمون تركيزات بلازما مواد الفضلات كرياتينين ويوريا (U)، وكذلك electrolytes (E) to determine renal function. These measures are adequate to determine whether a patient is suffering from kidney disease.
Unfortunately, blood urea nitrogen (BUN) and creatinine will not be raised above the normal range until 60% of total kidney function is lost. Hence, the more accurate Glomerular filtration rate or its approximation of the creatinine clearance are measured whenever renal disease is suspected or careful dosing of nephrotoxic drugs is required.
Another prognostic marker for kidney disease is an elevated level of protein in the urine. The most sensitive marker of proteinuria is elevated urine albumin. Persistence presence of more than 30 mg albumin per gram creatinine in the urine is diagnostic of chronic kidney disease (Microalbuminuria is a level of 30-299 mg/g; a concentration of albumin in the urine that is not detected by usual urine dipstick methods).
الرشح الكبي
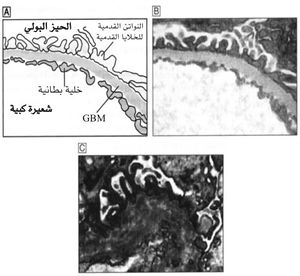
يدعى السائل الراشح من الكبيبات إلى محفظة بومان ب الرشاحة الكبية ،بينما يسمى غشاء الشعيرات الكبية ب الغشاء الكبي ، ورغم التشابه بين الغشاء الكبي وباقي أغشية الجسم عموماً إلا أنه توجد فروق عديدة حيث يحوي ثلاث طبقات رئيسة:
1-الطبقة البطانية للوعاء الشعري نفسه.
2-الغشاء الكبي القاعدي GBM.
3-طبقة الخلايا الظهارية .
ولكن رغم هذا العدد من الطبقات فإن نفوذية الغشاء الكبي أكبر ب 100-500 ضعف من نفوذية شعيرات الجسم الأخرى.تنتج النفوذية الشديدة للغشاء الكبي عن بنيته الخاصة، فهناك آلاف الثقوب في الخلايا البطانية الشعرية التي تستر الكبة تدعى هذه الثقوب بالنوافذ، أما الغشاء القاعدي فمؤلف من شيكة من ألياف الكولاجين و السكريات البروتينية التي تترك بينها فراغات واسعة يرشح السائل من خلالها.كما يوجد أيضاً مسافات بين الخلايا الظهارية ، التي هي آخر طبقة في بناء الغشاء وتستر السطح الخارجي للكبيبات.
هذا يعني أن الرشاحة الكبية تمر عبر ثلاث طبقات مختلفة قبل دخولها محفظة بومان وجميع هذه الطبقات سميمة(ذات مسام) أكثر بمئات الأضعاف من عدد المسام الموجودة في الأغشية الشعرية العادية، ولذلك تستطيع الكميات الضخمة من الرشاحة الكبية أن تعبر هذه الأغشية في كل دقيقة . وعلى الرغم من هذه النفوذية الهائلة للغشاء الكبي، فهو يمتلك أيضاً قدرة عالية جداً على انتخاب حجوم الجزيئات التي يسمح لها بالعبور.
وفيما يلي تقدير لنفوذية الغشاء الكبيبي للمواد ذات الأوزان الجزيئية المختلفة بشكل تقريبي (يعبر عن ذلك بنسبة تركيز المادة المنحلة في الجهة التي رشحت إليها عبر الغشاء إلى نسبتها في الجهة الأخرى للغشاء أي في المصورة).
| المادة | الوزن الجزيئي | النفوذية |
|---|---|---|
| الماء | 18 | 1 |
| الصوديوم | 23 | 1 |
| الگلوكوز | 180 | 1 |
| الأينولين | 5500 | 1 |
| الميوگلوبين | 17000 | 0.75 |
| الألبومين | 69000 | 0.005 |
يوجد سببان رئيسان لقدرة الانتخاب الجزئية العالية التي يتمتع بها الغشاء الكبيبي:
1-حجم المسام الموجودة في الغشاء نفسه الذي يكفي لعبور جزيئات يصل قطرها حتى 8 نانومتر تقريباً (80 أنغستروم)،ومن المعلوم أن قطر جزيء الألبومين هو 6 نانومتر تقريباً ؛أي أقل من قطر المسام في الغشاء،ومع ذلك لا تعبر جزيئات البروتين هذه المسام بكمية كبيرة والسبب في ذلك يعود إلى العامل الثاني المحدد لنفوذية الغشاء :
2-إن أجزاء الغشاء القاعدي في المسام الكبية مغطاة بطبقة من مركب السكريات البروتينية التي تحمل شحنة كهربائية سلبية قوية جداً ، ومن المعروف أن بروتينات المصورة تحمل شحنة كهربائية سلبية قوية أيضاً ، وبذلك يحدث تدافع كهربي سكوني بين الجزيئات وجدران المسام مما يمنع عملياً عبور جزيئات البروتين.[2]
معدل الرشح الكبي
تطلق هذه التسمية على كمية الرشاحة الكبية المتشكلة في كل دقيقة في جميع النفرونات في كلا الكليتين ، وهي تساوي تقريباً 125 مل/دقيقة عند الشخص السوي وبذلك تكون كمية الرشاحة الكبية المتشكلة في اليوم تعادل 180 لتراً تقريباً ، يعاد امتصاص أكثر من 99% من هذه الرشاحة عند الأشخاص الأسوياء ويعبر الباقي مع البول.[3]
القياس باستخدام الانيولين
The GFR can be determined by injecting inulin into the plasma. Since inulin is neither reabsorbed nor secreted by the kidney after glomerular filtration, its rate of excretion is directly proportional to the rate of filtration of water and solutes across the glomerular filter. Compared to the MDRD formula, the inulin clearance slightly overestimates the glomerular function. In early stage renal disease, the inulin clearance may remain normal due to hyperfiltration in the remaining nephrons[4]. Incomplete urine collection is an important source of error in inulin clearance measurement.
Creatinine-based approximations of GFR
In clinical practice, however, creatinine clearance or estimates of creatinine clearance based on the serum creatinine level are used to measure GFR. Creatinine is produced naturally by the body (creatinine is a break-down product of creatine phosphate, which is found in muscle). It is freely filtered by the glomerulus, but also actively secreted by the peritubular capillaries in very small amounts such that creatinine clearance overestimates actual GFR by 10-20%. This margin of error is acceptable considering the ease with which creatinine clearance is measured. Unlike precise GFR measurements involving constant infusions of inulin, creatinine is already at a steady-state concentration in the blood and so measuring creatinine clearance is much less cumbersome. However, creatinine estimates of GFR have their limitations. All of the estimating equations depend on a prediction of the 24-hour creatinine excretion rate, which is a function of muscle mass. One of the equations, the Cockcroft and Gault equation (see below) does not correct for race, and it is known that African Americans, for example, both men and women, have a higher amount of muscle mass than Caucasians; hence, African Americans will have a higher serum creatinine level at any level of creatinine clearance. A common mistake made when just looking at serum creatinine is the failure to account for muscle mass. Hence, an older woman with a serum creatinine of 1.4 may actually have a moderately severe degree of renal insufficiency, whereas a young muscular male, particularly if African American, can have a normal level of renal function at this serum creatinine level. Creatinine-based equations should be used with caution in cachectic patients and patients with cirrhosis. They often have very low muscle mass and a much lower creatinine excretion rate than predicted by the equations below, such that a cirrhotic patient with a serum creatinine of 0.9 may have a moderately severe degree of renal insufficiency.
إزالة الكرياتينين CCr
One method of determining GFR from creatinine is to collect urine (usually for 24-hours) to determine the amount of creatinine that was removed from the blood over a given time interval. If one removes, say, 1440 mg in 24 hours, this is equivalent to removing 1 mg/min. If the blood concentration is 0.01 mg/mL (1 mg/dL), then one can say that 100 mL/min of blood is being "cleared" of creatinine, since to get 1 mg of creatinine, 100 mL of blood containing 0.01 mg/mL would need to have been cleared.
Creatinine clearance (CCr) is calculated from the creatinine concentration in the collected urine sample (UCr), urine flow rate (V), and the plasma concentration (PCr). Since the product of urine concentration and urine flow rate yields creatinine excretion rate, which is the rate of removal from the blood, creatinine clearance is calculated as removal rate per min (UCr×V) divided by the plasma creatinine concentration. This is commonly represented mathematically as
Example: A person has a plasma creatinine concentration of 0.01 mg/ml and in 1 hour produces 60ml of urine with a creatinine concentration of 1.25 mg/mL.
Commonly a 24 hour urine collection is undertaken, from empty-bladder one morning to the contents of the bladder the following morning, with a comparative blood test then taken. The urinary flow rate is still calculated per minute, hence:
To allow comparison of results between people of different sizes, the CCr is often corrected for the body surface area (BSA) and expressed compared to the average sized man as mL/min/1.73 m2. While most adults have a BSA that approaches 1.7 (1.6-1.9), extremely obese or slim patients should have their CCr corrected for their actual BSA.
- BSA can be calculated on the basis of weight and height.
The creatinine clearance is not widely done any more, due to the difficulty in assuring a complete urine collection. When doing such a determination, to assess the adequacy of a complete collection, one always calculates the amount of creatinine excreted over a 24-hour period. This amount varies with muscle mass, and is higher in young people vs. old, in blacks vs. whites, and in men vs. women. An unexpectedly low or high 24-h creatinine excretion rate voids the test. Nevertheless, in cases where estimates of creatinine clearance from serum creatinine are unreliable, creatinine clearance remains a useful test. These cases include "estimation of GFR in individuals with variation in dietary intake (vegetarian diet, creatine supplements) or muscle mass (amputation, malnutrition, muscle wasting), since these factors are not specifically taken into account in prediction equations."[5]
القيم المقدرة
A number of formulae have been devised to estimate GFR or Ccr values on the basis of serum creatinine levels.
Estimated creatinine clearance rate (eCCr) using Cockcroft-Gault formula
A commonly used surrogate marker for estimate of creatinine clearance is the Cockcroft-Gault formula, which in turn estimates GFR:[6] It is named after the scientists who first published the formula, and it employs serum creatinine measurements and a patient's weight to predict the creatinine clearance. [7][8] The formula, as originally published, is:
- This formula expects weight to be measured in kilograms and creatinine to be measured in mg/dL, as is standard in the USA. The resulting value is multiplied by a constant of 0.85 if the patient is female. This formula is useful because the calculations are simple and can often be performed without the aid of a calculator.
When serum creatinine is measured in µmol/L:
- Where Constant is 1.23 for men and 1.04 for women.
One interesting feature of the Cockcroft and Gault equation is that it shows how dependent the estimation of CCr is based on age. The age term is (140 - age). This means that a 20-year-old person (140-20 = 120) will have twice the creatinine clearance as an 80-year old (140-80 = 60) for the same level of serum creatinine (120 is twice as great as 60). The C-G equation also shows that a woman will have a 15% lower creatinine clearance than a man at the same level of serum creatinine.
Estimated GFR (eGFR) using Modification of Diet in Renal Disease (MDRD) formula
The most recently advocated formula for calculating the GFR is the one that was developed by the Modification of Diet in Renal Disease Study Group.[9] Most laboratories in Australia,[10] and The United Kingdom now calculate and report the MDRD estimated GFR along with creatinine measurements and this forms the basis of Chronic kidney disease#Staging.[11] The adoption of the automatic reporting of MDRD-eGFR has been widely criticised.[12][13][14]
The most commonly used formula is the "4-variable MDRD" which estimates GFR using four variables: serum creatinine, age, race, and gender.[15] The original MDRD used six variables with the additional variables being the blood urea nitrogen and albumin levels.[9] The equations have been validated in patients with chronic kidney disease; however both versions underestimate the GFR in healthy patients with GFRs over 60 mL/min.[16][17] The equations have not been validated in acute renal failure.
For creatinine in mg/dL:
For creatinine in µmol/L:
- Creatinine levels in µmol/L can be converted to mg/dL by dividing them by 88.4. The 32788 number above is equal to 186×88.41.154.
A more elaborate version of the MDRD equation also includes serum albumin and blood urea nitrogen (BUN) levels:
- Where the creatinine and blood urea nitrogen concentrations are both in mg/dL. The albumin concentration is in g/dL.
These MDRD equations are to be used only if the laboratory has NOT calibrated its serum creatinine measurements to isotope dilution mass spectroscopy (IDMS). When IDMS-calibrated serum creatinine is used (which is about 6% lower), the above equations should be multiplied by 175/186 or by 0.94086. See: [1]
Since these formulae do not adjust for body mass, they (relative to the Cockcroft-Gault formula) underestimate eGFR for heavy people and overestimate it for underweight people. (see Cockcroft-Gault formula above).
Estimated GFR (eGFR) using the CKD-EPI formula
The CKD-EPI (Chronic Kidney Disease Epidemiology Collaboration) formula was published in May 2009. It was developed in an effort to create a formula more accurate formula than the MDRD formula, especially when actual GFR is greater than 60 mL/min per 1.73 m2.
Researchers pooled data from multiple studies to develop and validate this new equation. They used 10 studies which included 8254 participants, randomly using 2/3 of the data sets for development and the other 1/3 for internal validation. 16 additional studies, which included 3896 participants, were used for external validation.
The CKD-EPI equation performed better than the MDRD (Modification of Diet in Renal Disease Study) equation, especially at higher GFR, with less bias and greater accuracy. When looking at NHANES (National Health and Nutrition Examination Survey) data, the median estimated GFR was 94.5 mL/min per 1.73 m2 vs. 85.0 mL/min per 1.73 m2, and the prevalence of chronic kidney disease was 11.5% versus 13.1%.
The CKD-EPI equation, expressed as a single equation, is:
where SCr is serum creatinine (mg/dL), k is 0.7 for females and 0.9 for males, a is -0.329 for females and -0.411 for males, min indicates the minimum of SCr/k or 1, and max indicates the maximum of SCr/k or 1.
A clearer version may be as follows:
For creatinine (IDMS calibrated) in mg/dL:
African American Female
If serum creatinine (Scr) <= 0.7
If serum creatinine (Scr) > 0.7
African American Male
If serum creatinine (Scr) <= 0.9
If serum creatinine (Scr) > 0.9
White or other race Female
If serum creatinine (Scr) <= 0.7
If serum creatinine (Scr) > 0.7
White or other race Male
If serum creatinine (Scr) <= 0.9
If serum creatinine (Scr) > 0.9
This formula was developed by Levey et al. [18]
The formula CKD-EPI may provide improved cardiovascular risk prediction over the MDRD Study formula in a middle age population(Matsushita K et al.).
Estimated GFR (eGFR) using the Mayo Quadratic formula
Another estimation tool to calculate GFR is the Mayo Quadratic formula. This formula was developed by Rule et al. [16] in an attempt to better estimate GFR in patients with preserved kidney function. It is well recognized that the MDRD formula tends to underestimate GFR in patients with preserved kidney function.
The equation is: GFR = exp(1.911 + 5.249/SCr - 2.114/Scr^2 - 0.00686 * Age -0.205 (if female))
If SCr < 0.8 mg/dL, use 0.8 for SCr
Estimated GFR for children using Schwartz formula
In children, the Schwartz formula is used.[19][20] This employs the serum creatinine (mg/dL), the child's height (cm) and a constant to estimate the glomerular filtration rate:
- Where k is a constant that depends on muscle mass, which itself varies with a child's age:
The method of selection of the K-constant value has been questioned as being dependent upon the gold-standard of renal function used (i.e. creatinine clearance, inulin clearance etc) and also may be dependent upon the urinary flow rate at the time of measurement.[22]
In 2009, the formula was updated to use standardized serum creatinine (recommend k=0.413) and additional formulas were derived which allow improved precision if serum cystatin measured in addition to serum creatinine.(Schwartz et al. 2009)
Importance of calibration of the serum creatinine level and the IDMS standardization effort
One problem with any creatinine-based equation for GFR is that the methods used to assay creatinine in the blood differ widely in their susceptibility to non-specific chromogens, which cause the creatinine value to be overestimated. In particular, the MDRD equation was derived using serum creatinine measurements which had this problem. The NKDEP program in the United States has attempted to solve this problem by trying to get all laboratories to calibrate their measures of creatinine to a "gold standard", which in this case is isotope dilution mass spectroscopy (IDMS). At the present time in late 2009 not all labs in the U.S. have changed over to the new system. There are two forms of the MDRD equation that are available, depending on whether or not creatinine was measured by an IDMS-calibrated assay. The CKD-EPI equation is designed to be used with IDMS-calibrated serum creatinine values only.
Cystatin C
Problems with creatinine (varying muscle mass, recent meat ingestion, etc.) have led to evaluation of alternative agents for estimation of GFR. One of these is cystatin C, a ubiquitous protein secreted by most cells in the body (it is an inhibitor of cysteine protease) that is freely filtered at the glomerulus and not reabsorbed. After filtration, cystatin C is normally catabolized in the renal tubules and none appears in the urine, so urine collection methods cannot be used. However, equations have been developed linking estimated GFR to serum cystatin C levels. Most recently (2009) some proposed equations have combined creatinine and cystatin.
Normal ranges
The normal range of GFR, adjusted for body surface area, is similar in men and women, and is in the range of 100-130 ml/min/1.73m2. In children, GFR measured by inulin clearance remains close to about 110 ml/min/1.73m2 down to about 2 years of age in both sexes, and then it progressively decreases. After age 40, GFR decreases progressively with age, by about 0.4 - 1.2 mL/min per year.
Chronic kidney disease stages
Risk factors for kidney disease include diabetes, high blood pressure, family history, older age, ethnic group and smoking. For most patients, a GFR over 60 mL/min/1.73m2 is adequate. But, if the GFR has significantly declined from a previous test result, this can be an early indicator of kidney disease requiring medical intervention. The sooner kidney dysfunction is diagnosed and treated, the greater odds of preserving remaining nephrons, and preventing the need for dialysis.
The severity of chronic kidney disease (CKD) is described by six stages; the most severe three are defined by the MDRD-eGFR value, and first three also depend whether there is other evidence of kidney disease (e.g. proteinuria):
- 0) Normal kidney function – GFR above 90mL/min/1.73m2 and no proteinuria
- 1) CKD1 – GFR above 90mL/min/1.73m2 with evidence of kidney damage
- 2) CKD2 (Mild) – GFR of 60 to 89 mL/min/1.73m2 with evidence of kidney damage
- 3) CKD3 (Moderate) – GFR of 30 to 59 mL/min/1.73m2
- 4) CKD4 (Severe) – GFR of 15 to 29 mL/min/1.73m2
- 5) CKD5 Kidney failure - GFR less than 15 mL/min/1.73m2 Some people add CKD5D for those stage 5 patients requiring dialysis; many patients in CKD5 are not yet on dialysis.
Note: others add a "T" to patients who have had a transplant regardless of stage.
Controversies regarding the KDOQI classification
One problem with the KDOQI classification is, that it may overlabel patients with mildly reduced kidney function, especially the elderly, as having a disease. See [2] for a review of these issues by Bauer et al. and also a recent KDIGO/KDOQI position statement here: [3]. Kidney Disease: Improving Global Outcomes (KDIGO) held a controversies conference in 2009 on CKD: Definition, Classification and Prognosis which gathered data on CKD prognosis to refine the definition and staging of CKD.
انظر أيضا
- Clearance
- Dialysis
- filtration fraction
- Kt/V
- Pharmacokinetics
- Renal clearance ratio
- فشل كلوي
- Standardized Kt/V
- Tubuloglomerular feedback
- Urea reduction ratio
المصادر
- ^ Stevens LA, Coresh J, Greene T, Levey AS. Assessing kidney function--measured and estimated glomerular filtration rate. N Engl J Med. 2006 Jun 8;354(23):2473-83.
- ^ أمل ركاج :"الفيزيولوجيا"منشورات جامعة دمشق ،كلية الصيدلة
- ^ أمل ركاج :"الفيزيولوجيا"منشورات جامعة دمشق ،كلية الصيدلة
- ^ GFR (Cockcroft & MDRD) calculator at medical-calculator.nl - Cockcroft and MDRD calculator and details about inulin clearance
- ^ National Kidney Foundation KDOQI GUIDELINES http://www.kidney.org/professionals/kdoqi/guidelines_ckd/p5_lab_g4.htm
- ^ GFR Calculator at cato.at - Cockcroft-Gault - GFR calculation (Cockcroft-Gault formula)
- ^ Cockcroft DW, Gault MH (1976). "Prediction of creatinine clearance from serum creatinine". Nephron. 16 (1): 31–41. doi:10.1159/000130554. PMID 1244564.
- ^ Gault MH, Longerich LL, Harnett JD, Wesolowski C (1992). "Predicting glomerular function from adjusted serum creatinine". Nephron. 62 (3): 249–56. doi:10.1159/000187054. PMID 1436333.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ أ ب Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D (1999). "A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of Diet in Renal Disease Study Group" (PDF). Ann. Intern. Med. 130 (6): 461–70. PMID 10075613.
{{cite journal}}: CS1 maint: multiple names: authors list (link) خطأ استشهاد: وسم<ref>غير صالح؛ الاسم "pmid10075613" معرف أكثر من مرة بمحتويات مختلفة. - ^ Mathew TH, Johnson DW, Jones GR (2007). "Chronic kidney disease and automatic reporting of estimated glomerular filtration rate: revised recommendations". Med. J. Aust. 187 (8): 459–63. PMID 17937643.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Joint Specialty Committee on Renal Disease (2005). "Chronic kidney disease in adults: UK guidelines for identification, management and referral" (PDF).
{{cite web}}: Unknown parameter|month=ignored (help) - ^ Davey RX (2006). "Chronic kidney disease and automatic reporting of estimated glomerular filtration rate". Med. J. Aust. 184 (1): 42–3, author reply 43. PMID 16398632.
- ^ Twomey PJ, Reynolds TM (2006). "The MDRD formula and validation". QJM. 99 (11): 804–5. doi:10.1093/qjmed/hcl108. PMID 17041249.
- ^ Kallner A, Ayling PA, Khatami Z (2008). "Does eGFR improve the diagnostic capability of S-Creatinine concentration results? A retrospective population based study". Int J Med Sci. 5 (1): 9–17. PMC 2204044. PMID 18219370.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ National Kidney, Foundation (2002). "K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification". Am. J. Kidney Dis. 39 (2 Suppl 1): S1–266. PMID 11904577.
- ^ أ ب Rule AD, Larson TS, Bergstralh EJ, Slezak JM, Jacobsen SJ, Cosio FG (2004). "Using serum creatinine to estimate glomerular filtration rate: accuracy in good health and in chronic kidney disease". Ann. Intern. Med. 141 (12): 929–37. PMID 15611490.
{{cite journal}}: CS1 maint: multiple names: authors list (link) خطأ استشهاد: وسم<ref>غير صالح؛ الاسم "pmid15611490" معرف أكثر من مرة بمحتويات مختلفة. - ^ Levey AS, Coresh J, Greene T; et al. (2006). "Using standardized serum creatinine values in the modification of diet in renal disease study equation for estimating glomerular filtration rate". Ann. Intern. Med. 145 (4): 247–54. PMID 16908915.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF 3rd, Feldman HI, Kusek JW, Eggers P, Van Lente F, Greene T, Coresh J. (2009). "A new equation to estimate glomerular filtration rate". Ann. Intern. Med. 150 (9): 604–12. PMC 2763564. PMID 19414839.
{{cite journal}}: CS1 maint: multiple names: authors list (link) CS1 maint: numeric names: authors list (link) - ^ أ ب Schwartz GJ, Haycock GB, Edelmann CM, Spitzer A (1976). "A simple estimate of glomerular filtration rate in children derived from body length and plasma creatinine". Pediatrics. 58 (2): 259–63. PMID 951142.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ أ ب Schwartz GJ, Feld LG, Langford DJ (1984). "A simple estimate of glomerular filtration rate in full-term infants during the first year of life". J. Pediatr. 104 (6): 849–54. doi:10.1016/S0022-3476(84)80479-5. PMID 6726515.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Brion LP, Fleischman AR, McCarton C, Schwartz GJ (1986). "A simple estimate of glomerular filtration rate in low birth weight infants during the first year of life: noninvasive assessment of body composition and growth". J. Pediatr. 109 (4): 698–707. doi:10.1016/S0022-3476(86)80245-1. PMID 3761090.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Haenggi MH, Pelet J, Guignard JP (1999). "[Estimation of glomerular filtration rate by the formula GFR = K x T/Pc]". Arch Pediatr (in French). 6 (2): 165–72. doi:10.1016/S0929-693X(99)80204-8. PMID 10079885.
{{cite journal}}: CS1 maint: multiple names: authors list (link) CS1 maint: unrecognized language (link)
وصلات خارجية
Cockcroft-Gault calculators
- Online GFR Calculator (Cockcroft-Gault Formula)
- Online calculator for Cockcroft-Gault and MDRD formulae.
MDRD calculators
- Online calculator for Cockcroft-Gault and MDRD formulae.
Cockcroft - Gault / MDRD Combination Calculators
- Online GFR Calculator utilizing the Cockcroft-Gault formula, the MDRD formula, and a combination of both formulas.
Calculator also computes the expected GFR for age and the percentage of the patient's current GFR as compared to normal.
Other formulas calculators
وصلات مراجع
- National Kidney Disease Education Program website. Includes professional references and GFR calculators




![{\displaystyle eC_{Cr}={\frac {{\mbox{(140 - Age)}}\ \times \ {\mbox{Mass (in kilograms)}}\ \times \ [{0.85\ if\ Female}]}{{\mbox{72}}\ \times \ {\mbox{Serum Creatinine (in mg/dL)}}}}}](https://wikimedia.org/api/rest_v1/media/math/render/svg/e0f25bf7dd65347e62a6b5a47c3f5fbb15a31817)

![{\displaystyle {\mbox{eGFR}}={\mbox{186}}\ \times \ {\mbox{Serum Creatinine}}^{-1.154}\ \times \ {\mbox{Age}}^{-0.203}\ \times \ {[1.210\ if\ Black]}\ \times \ {[0.742\ if\ Female]}}](https://wikimedia.org/api/rest_v1/media/math/render/svg/4af038a35b898c5f50b387c5d5f25d11ca8e78e2)
![{\displaystyle {\mbox{eGFR}}={\mbox{32788}}\ \times \ {\mbox{Serum Creatinine}}^{-1.154}\ \times \ {\mbox{Age}}^{-0.203}\ \times \ {[1.210\ if\ Black]}\ \times \ {[0.742\ if\ Female]}}](https://wikimedia.org/api/rest_v1/media/math/render/svg/f030f594a4914d1da4694ab1c9d9650c1da0e7a1)
![{\displaystyle {\mbox{eGFR}}={\mbox{170}}\ \times \ {\mbox{Serum Creatinine}}^{-0.999}\ \times \ {\mbox{Age}}^{-0.176}\ \times \ {[0.762\ if\ Female]}\ \times \ {[1.180\ if\ Black]}\ \times \ {\mbox{BUN}}^{-0.170}\ \times \ {\mbox{Albumin}}^{+0.318}}](https://wikimedia.org/api/rest_v1/media/math/render/svg/42123f9a84e1de6b97e37100b2831ac063db6e46)
![{\displaystyle {\mbox{eGFR}}={\mbox{141}}\ \times \ {\mbox{min(SCr/k,1)}}^{a}\ \times \ {\mbox{max(SCr/k,1)}}^{-1.209}\ \times \ {\mbox{0.993}}^{Age}\ \times \ {[1.018\ if\ Female]}\ \times \ {[1.159\ if\ Black]}\ }](https://wikimedia.org/api/rest_v1/media/math/render/svg/1a67dbd5402860c929af2716c6474a7b514b92f6)








