سرطان الكلية
| Kidney cancer | |
|---|---|
| الأسماء الأخرى | Renal cancer |
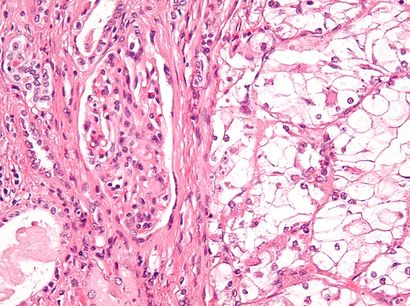 | |
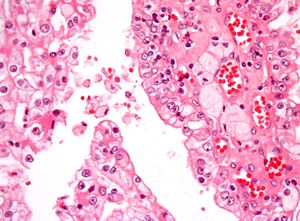
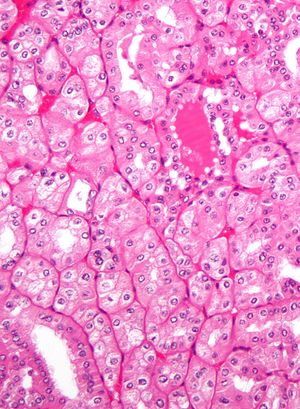
| Micrograph showing the most common type of kidney cancer (clear cell renal cell carcinoma). H&E stain. | |
| التخصص | Oncology, nephrology |
| الأعراض | Blood in the urine, lump in the abdomen, back pain[1][2][3] |
| البداية المعتادة | After the age of 45[4] |
| الأنواع | Renal cell carcinoma (RCC), transitional cell carcinoma (TCC), Wilms tumor[4] |
| عوامل الخطر | Smoking, certain pain medications, previous bladder cancer, being overweight, high blood pressure, certain chemicals, family history[1][2] |
| الطريقة التشخيصية | Tissue biopsy[1][2][3] |
| العلاج | Surgery, radiation therapy, chemotherapy, immunotherapy, targeted therapy[1][2][3] |
| Prognosis | Five-year survival ~75% (US 2015)[4] |
| التردد | 403,300 (2018)[5] |
| الوفيات | 175,000[5] |
سرطان الكلية إنگليزية: Kidney cancer هي الأورام التي تنشأ من أنسجة الكلية وهنالك نوعان رئيسان لهذا السرطان مصنفان بحسب منشئهما النسيجي و هما:
- سرطانة الخلايا الكلوية إنگليزية: renal cell carcinoma.
- سرطانة حويضة الكلية إنگليزية: renal pelvis carcinoma.
يتوجب التفريق بين منشأ النوعين عند التعامل مع السرطان و ذلك لأن لكل نوع مزايا خاصة تأثر على خيارات العلاج. تنشأ السرطانات قي الكلية إما من الكليونات أو من حويضة الكلية، أهم سرطانات الكليونات: سرطانة الخلايا الكلوية والسرطانة الغدية ذات الخلايا الصافية إنگليزية: Clear cell adenocarcinoma، أما أكثر سرطانات حويضة الكلية شيوعاً فهي سرطانة الخلايا الانتقالية إنگليزية: Transitional cell carcinoma.
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
أنواع سرطانات الكلية
بالإضافة لسرطانة الخلايا الكلوية و سرطانة حويضة الكلية، فإن هنالك أنواعاً أخرى من السرطان تصيب الكلية ولكنها ندارة نسبياً، من هذه الأنواع:
- سرطان الخلايا الحرشفية إنگليزية: Squamous cell carcinoma
- ورم رينيني إنگليزية: Reninoma
- ورم شحمي عضلي وعائي كلوي إنگليزية: Renal angiomyolipoma
- ورم أورمي كلوي (ورم ويلم) إنگليزية: Nephroblastoma
الأعراض
من الأعراض الشائعة المصاحبة لسرطانات الكلية ما يلي:
- وجود كتلة في التجويف البطني (يتم اكتشافها عن طريق الجس)، وهي أكثر الأعراض شيوعاً [6]، ويتم جسها عادة في الناحية القطنية الأمامية.
- بيلة دموية إنگليزية: Hematuria.
- موه الكلية إنگليزية: Hydronephrosis.
كما يمكن أن ينشأ السرطان دون أية أعراض تذكر ولكن ذلك قليل الحدوث. وقد تم حديثا اكتشاف أن توضع القولون يشكل علامة دالة في تشخيص سرطانات الكلية.[6]
المسببات
Factors that increase the risk of kidney cancer include smoking, which can double the risk of the disease; obesity; faulty genes; a family history of kidney cancer; having kidney disease that needs dialysis; being infected with hepatitis C; and previous treatment for testicular cancer or cervical cancer.
There are also other possible risk factors such as kidney stones[7] and high blood pressure, which are being investigated.[8] Some studies have linked regular use of NSAIDs such as ibuprofen and naproxen to increases of kidney cancer risk by up to 51%.
التشخيص
التبويب
Kidney masses can be classified by the nature of the cells in the growth, or by its appearance on radiography.[9] The term cancer refers to a malignant tumor, which is an uncontrolled growth of abnormal cells.[10] However, kidney masses can be due to growth of normal tissue (benign), inflammatory (a reaction of the immune system), or vascular (cells of the blood vessels). Radiologically tumors are grouped based on appearance into simple cystic, complex cystic, or solid.[9]
The most common type of kidney malignancy is renal cell carcinoma,[11] which is thought to originate from cells in the proximal convoluted tubule of the nephron.[9][12] Another type of kidney cancer although less common, is transitional cell cancer (TCC) or urothelial carcinoma of the renal pelvis.[13] The renal pelvis is the part of the kidney that collects urine and drains it into a tube called the ureter.[13] The cells that line the renal pelvis are called transitional cells, and are also sometimes called urothelial cells. The transitional/urothelial cells in the renal pelvis are the same type of cells that line the ureter and bladder. For this reason TCC of the renal pelvis is distinct from RCC and is thought to behave more like bladder cancer.[13] Other rare types of kidney cancers that can arise from the urothelial cells of the renal pelvis are squamous cell carcinoma and adenocarcinoma.[9]
Other causes of kidney cancer include the following:[9]
- Sarcoma- for example leiomyosarcoma, liposarcoma, angiosarcoma, clear-cell sarcoma and rhabdomyosarcoma are types of sarcomas that have occurred in the kidney
- Metastatic tumor from distant organ
- Lymphoma
- Wilms tumor- an embryonic tumor that is the most common type of kidney cancer in children
- Carcinoid tumor of the renal pelvis[14]
- Carcinosarcoma[15]
- Inverted urothelial papilloma- was traditionally regarded as a benign growth. However, there may be an increased risk for recurrence and transformation to TCC.[16]
In children, Wilms tumor is the most common type of kidney cancer.[9] Mesoblastic nephroma, although rare, also typically presents in childhood.
Renal cell carcinoma has been further divided into sub-types based on histological features and genetic abnormalities. The 2004 WHO Classification of the Renal Tumors of the Adults describes these categories:[17]
- Clear cell RCC
- Multilocular clear cell RCC
- Papillary RCC
- Chromophobe RCC
- Carcinoma of the collecting ducts of Bellini
- Renal medullary carcinoma
- Xp11 translocation carcinoams
- Carcinoma associated with neuroblastoma
- Mucinous tubular and spindle cell carcinoma
- Mixed epithelial stromal tumor[18]
Tumors that are considered benign include angiomyolipoma, oncocytoma, reninoma (juxtaglomerular cell tumor), and renal adenoma.[9]
التصوير الطبي
Since there is a large differential diagnosis for a kidney tumor, the first step is to characterize the mass with medical imaging to assess the likelihood of a benign or malignant nature. Ultrasonography is sometimes used to evaluate a suspected kidney mass, as it can characterize cystic and solid kidney masses without radiation exposure and at relative low cost.[9] Simple cysts, which are defined by strict criteria[19] are safe to be monitored if the person does not have any symptoms.[9] However, all masses that are not clearly simple cysts should be further evaluated and confirmed by alternate imaging techniques.[20][9]
Computed tomography (CT) of the abdomen administered with and without IV contrast is the ideal imaging to diagnose and stage kidney cancer.[21][20][9] There is tentative evidence that iodinated contrast agents may cause worsening of kidney function in people with chronic kidney disease (CKD) with a glomerular filtration rate (GFR) less than 45ml/min/1.73m2 and should therefore be given cautiously in this group.[22]
Abdominal magnetic resonance imaging (MRI) is an alternative imaging method that can be used to characterize and stage a kidney mass.[23][20][9] It may be suggested if contrast material cannot be given.[23] MRI can also evaluate the inferior vena cava if the mass is suspected to extend outside the kidney.[23]
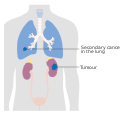
Since the lungs are the most common organ for kidney cancer to spread to, a chest X-ray or CT scan may be ordered based on the person’s risk for metastatic disease.[9][20]
الدراسات المعملية
People with suspected kidney cancer should also have their kidney function evaluated to help determine treatment options. Blood tests to determine kidney function include a comprehensive metabolic panel (CMP), a complete blood count (CBC).[24][20] In addition, these tests help understand the overall health of the person, which can be affected by metastatic disease (disease that is outside of the kidney). For example, liver or bone involvement could result in abnormal liver enzymes, electrolyte abnormalities, or anemia. A urine sample should also be collected for urinalysis.[20][9]
خزعة
The utility of renal mass biopsy (RMB) lies in that it can confirm malignancy with reliability, can direct therapy based on diagnosis, and can provide drainage.[20]
Once imaging has been completed, renal mass biopsy should be considered if there is a high likelihood that the mass is hematologic, metastatic, inflammatory, or infectious.[20] These types of lesions would not be managed surgically, differing from cancer originating from the kidney. Cancer originating outside the kidney and lymphoma are managed systemically.[9][20]
RMB can accurately diagnose malignancy, however, it cannot reliably diagnose benign disease. In other words, if the biopsy shows cancer, there is a 99.8% chance that kidney cancer is present (Positive Predictive Value= 99.8%). A negative biopsy does not rule out a diagnosis of cancer.[25]
المراحل
Staging is the process the process that helps determine the extent and spread of the disease.[26] Renal cell carcinoma is the only type of kidney cancer that can be staged. The first step of staging follows the TNM staging system proposed by the Union International Contre le Cancer that is widely used among cancers in other organs.[9] The TNM staging system classifies the primary tumor (T), lymph nodes (N) and distant metastasis (M) of the disease. The American Joint Committee on Cancer (AJCC) published a Cancer Staging Manual revision in 2010 that describes the values of TMN for renal cell carcinoma.[27][9]
Lymph node involvement is classified as either regional lymph node metastasis (N1), or no involvement (N0).[27] Similarly, M1 describes distant metastasis, while M0 describes no distant metastasis.[27]
The primary tumor of renal cell carcinoma is categorized in the table below, as according to the AJCC 2010 7th Edition Cancer Staging Manual.[27]
| Tx | Tumor cannot be assessed |
| T0 | No evidence of primary tumor |
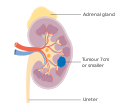
| T1 | Tumor ≤7 cm; limited to kidney |
| T1a | Tumor ≤4 cm; limited to kidney |
| T1b | Tumor 4-≤7 cm; limited to kidney |
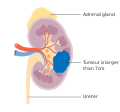
| T2 | Tumor >7 cm; limited to kidney |
| T2a | Tumor 7-≤10 cm; limited to kidney |
| T2b | Tumor >10 cm; limited to kidney |
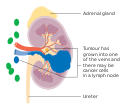
| T3 | Tumor extends to major veins or perinephric tissue but not into ipsilateral adrenal gland nor beyond Gerota's fascia |
| T3a | Tumor grossly extends into renal vein or its' segmental branches, or tumor invades perirenal and/or renal sinus fat but not beyond Gerota's fascia |
| T3b | Tumor grossly extends into vena cava below the diaphragm |
| T3c | Tumor grossly extends into vena cava above the diaphragm or invades the wall of the vena cava |
| T4 | Tumor invvades beyond Gerota's fascia |
Once the cancer is described by the TNM staging system, the anatomic stage can be determined, which aides physicians in understanding prognosis.[9] The more advanced the disease the higher the number stage.[28] Renal Cell Carcinoma that is deemed metastatic is by definition Stage IV kidney cancer.[27] The lungs are the most common site for metastasis ,[20] with other common sites including bone, brain, liver, adrenal gland and distant lymph nodes.[29][28][27] Below is the AJCC 2010 7th Edition Cancer Staging Manual Staging classification.[27]
| Tumor (T) | Lymph Node (N) | Metastasis (M) | |
| Stage I | T1 | N0 | M0 |
| Stage II | T2 | N0 | M0 |
| Stage III | T1 or T2
T3 |
N1
N0 or N1 |
M0
M0 |
| Stage IV | T4
Any T |
Any N
Any N |
M0
M1 |
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
العلاج
Treatment for kidney cancer depends on the type and stage of the disease. Surgery is the most common treatment as kidney cancer does not often respond to chemotherapy and radiotherapy. Surgical complexity can be estimated by the RENAL Nephrometry Scoring System. If the cancer has not spread it will usually be removed by surgery. In some cases this involves removing the whole kidney however most tumors are amenable to partial removal to eradicate the tumor and preserve the remaining normal portion of the kidney. Surgery is not always possible – for example the patient may have other medical conditions that prevent it, or the cancer may have spread around the body and doctors may not be able to remove it.[30] There is currently no evidence that body-wide medical therapy after surgery where there is no known residual disease, that is, adjuvant therapy, helps to improve survival in kidney cancer. If the cancer cannot be treated with surgery other techniques such as freezing the tumour or treating it with high temperatures may be used. However these are not yet used as standard treatments for kidney cancer.[31]
Other treatment options include biological therapies such as everolimus, torisel, nexavar, sutent, and axitinib, the use of immunotherapy including interferon and interleukin-2.[32][33][34] Immunotherapy is successful in 10 to 15% of people.[35] Sunitinib is the current standard of care in the adjuvant setting along with pazopanib; these treatments are often followed by everolimus, axitinib, and sorafenib. Immune checkpoint inhibitors are also in trials for kidney cancer, and some have gained approval for medical use.[36]
In the second line setting, nivolumab demonstrated an overall survival advantage in advanced clear renal cell carcinoma over everolimus in 2015 and was approved by the FDA.[36][37] Cabozantinib also demonstrated an overall survival benefit over everolimus and was approved by the FDA as a second-line treatment in 2016.[38][39][40] Lenvatinib in combination with everolimus was approved in 2016 for patients who have had exactly one prior line of angiogenic therapy.[41]
In Wilms' tumor, chemotherapy, radiotherapy and surgery are the accepted treatments, depending on the stage of the disease when it is diagnosed.[42]
الأطفال
The majority of kidney cancers reported in children are Wilms' tumors. These tumors can begin to grow when a fetus is still developing in the uterus, and may not cause problems until the child is a few years old. Wilms' tumor is most common in children under the age of 5, but can rarely be diagnosed in older children or in adults. It is still not clear what causes most Wilms' tumors. The most common symptoms are swelling of the abdomen and blood in the urine.[42]
الوبائيات
تشخص سنوياً أكثر من 208,500 حالة سرطان كلية حول العالم، وتشكل سرطانات الكلية ما نسبته 2% من مجموع السرطانات التي تصيب الإنسان [43]. لوحظ أن أعلى معدلات الإصابة هو في أمريكا الشمالية و أن أقلها في آسيا وأفريقيا [44]. في 2008 شخصت 54,390 حالة إصابة جديدة في الولايات المتحدة أوقعت 13,010 وفية [45] . بعض سرطانات الكلى تسري في العائلات و تورث جينياً [46] بينما البعض الآخر يرتبط حدوثه بعوامل اختطار خارجية كالتدخين والتعرض للمواد المسرطنة.
أنظر أيضا
مراجع
- ^ أ ب ت ث خطأ استشهاد: وسم
<ref>غير صحيح؛ لا نص تم توفيره للمراجع المسماةNCI2019RCC - ^ أ ب ت ث خطأ استشهاد: وسم
<ref>غير صحيح؛ لا نص تم توفيره للمراجع المسماةNCI2019TCC - ^ أ ب ت خطأ استشهاد: وسم
<ref>غير صحيح؛ لا نص تم توفيره للمراجع المسماةNCI2019Wl - ^ أ ب ت خطأ استشهاد: وسم
<ref>غير صحيح؛ لا نص تم توفيره للمراجع المسماةSEER2019 - ^ أ ب خطأ استشهاد: وسم
<ref>غير صحيح؛ لا نص تم توفيره للمراجع المسماةIARC2018 - ^ أ ب William Roberts and Robert Maguire (1885). A practical treatise on urinary and renal diseases (4th ed.). Smith, Elder and Co. p. 697.
{{cite book}}: Unknown parameter|address=ignored (|location=suggested) (help), page 581 - ^ Cheungpasitporn, W; Thongprayoon C; O'Corragain OA; Edmonds PJ; Ungprasert P; Kittanamongkolchai W; Erickson SB (9 September 2014). "The Risk of Kidney Cancer in Patients with Kidney Stones: A Systematic Review and Meta-analysis". QJM. 108 (3): 205–12. doi:10.1093/qjmed/hcu195. PMID 25208892.
- ^ "Risks and causes of kidney cancer". 2017-08-30.
- ^ أ ب ت ث ج ح خ د ذ ر ز س ش ص ض ط ظ ع خطأ استشهاد: وسم
<ref>غير صحيح؛ لا نص تم توفيره للمراجع المسماة:07 - ^ "Cancer | Definition of Cancer by Lexico". Lexico Dictionaries | English. Retrieved 2019-11-12.
- ^ "Kidney Cancer | CDC". www.cdc.gov. 2019-07-09. Retrieved 2019-11-12.
- ^ "Renal Cell Cancer Treatment (PDQ®)–Patient Version". National Cancer Institute. 2004-02-20. Retrieved 2019-11-12.
- ^ أ ب ت "Transitional Cell Cancer of the Renal Pelvis and Ureter Treatment (PDQ®)–Patient Version". National Cancer Institute. 2004-02-20. Retrieved 2019-11-12.
- ^ Kuroda N, Katto K, Tamura M, Shiotsu T, Hes O, Michal M, Nagashima Y, Ohara M, Hirouchi T, Mizuno K, Hayashi Y, Lee GH (January 2008). "Carcinoid tumor of the renal pelvis: consideration on the histogenesis". Pathol. Int. 58 (1): 51–4. doi:10.1111/j.1440-1827.2007.02188.x. PMID 18067641.
- ^ Chiu, KC; Lin, MC; Liang, YC; Chen, CY (2008). "Renal carcinosarcoma: case report and review of literature". Renal Failure. 30 (10): 1034–9. doi:10.1080/08860220802403192. PMID 19016157.
- ^ Picozzi, Stefano; Casellato, Stefano; Bozzini, Giorgio; Ratti, Dario; Macchi, Alberto; Rubino, Barbara; Pace, Gianna; Carmignani, Luca (November 2013). "Inverted papilloma of the bladder: a review and an analysis of the recent literature of 365 patients". Urologic Oncology. 31 (8): 1584–1590. doi:10.1016/j.urolonc.2012.03.009. ISSN 1873-2496. PMID 22520573.
- ^ Lopez-Beltran, Antonio; Scarpelli, Marina; Montironi, Rodolfo; Kirkali, Ziya (May 2006). "2004 WHO classification of the renal tumors of the adults". European Urology. 49 (5): 798–805. doi:10.1016/j.eururo.2005.11.035. ISSN 0302-2838. PMID 16442207.
- ^ Thyavihally YB, Tongaonkar HB, Desai SB (September 2005). "Benign mixed epithelial stromal tumor of the renal pelvis with exophytic growth: case report". Int Semin Surg Oncol. 2: 18. doi:10.1186/1477-7800-2-18. PMC 1215508. PMID 16150156.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Silverman, Stuart G.; Pedrosa, Ivan; Ellis, James H.; Hindman, Nicole M.; Schieda, Nicola; Smith, Andrew D.; Remer, Erick M.; Shinagare, Atul B.; Curci, Nicole E.; Raman, Steven S.; Wells, Shane A. (2019-06-18). "Bosniak Classification of Cystic Renal Masses, Version 2019: An Update Proposal and Needs Assessment". Radiology. 292 (2): 475–488. doi:10.1148/radiol.2019182646. ISSN 0033-8419.
- ^ أ ب ت ث ج ح خ د ذ ر "Renal Cancer: Renal Mass & Localized Renal Cancer Guideline - American Urological Association". www.auanet.org. Retrieved 2019-10-29.
- ^ Motzer, Robert J.; Jonasch, Eric; Agarwal, Neeraj; Bhayani, Sam; Bro, William P.; Chang, Sam S.; Choueiri, Toni K.; Costello, Brian A.; Derweesh, Ithaar H.; Fishman, Mayer; Gallagher, Thomas H. (2017-06-01). "Kidney Cancer, Version 2.2017, NCCN Clinical Practice Guidelines in Oncology". Journal of the National Comprehensive Cancer Network. 15 (6): 804–834. doi:10.6004/jnccn.2017.0100. ISSN 1540-1405.
- ^ Subramaniam, Rathan M.; Wilson, Renee F.; Turban, Sharon; Suarez-Cuervo, Catalina; Zhang, Allen; Sherrod, Cheryl; Aboagye, Jonathan; Eng, John; Choi, Michael J. (2016). Contrast-Induced Nephropathy: Comparative Effectiveness of Preventive Measures. AHRQ Comparative Effectiveness Reviews. Rockville (MD): Agency for Healthcare Research and Quality (US). PMID 26866209.
- ^ أ ب ت Motzer, Robert J.; Jonasch, Eric; Agarwal, Neeraj; Bhayani, Sam; Bro, William P.; Chang, Sam S.; Choueiri, Toni K.; Costello, Brian A.; Derweesh, Ithaar H.; Fishman, Mayer; Gallagher, Thomas H. (2017-06-01). "Kidney Cancer, Version 2.2017, NCCN Clinical Practice Guidelines in Oncology". Journal of the National Comprehensive Cancer Network. 15 (6): 804–834. doi:10.6004/jnccn.2017.0100. ISSN 1540-1405.
- ^ Motzer, Robert J.; Jonasch, Eric; Agarwal, Neeraj; Bhayani, Sam; Bro, William P.; Chang, Sam S.; Choueiri, Toni K.; Costello, Brian A.; Derweesh, Ithaar H.; Fishman, Mayer; Gallagher, Thomas H. (2017-06-01). "Kidney Cancer, Version 2.2017, NCCN Clinical Practice Guidelines in Oncology". Journal of the National Comprehensive Cancer Network. 15 (6): 804–834. doi:10.6004/jnccn.2017.0100. ISSN 1540-1405.
- ^ Patel, Hiten D.; Johnson, Michael H.; Pierorazio, Phillip M.; Sozio, Stephen M.; Sharma, Ritu; Iyoha, Emmanuel; Bass, Eric B.; Allaf, Mohamad E. (May 2016). "Diagnostic Accuracy and Risks of Biopsy in the Diagnosis of a Renal Mass Suspicious for Localized Renal Cell Carcinoma: Systematic Review of the Literature". The Journal of Urology. 195 (5): 1340–1347. doi:10.1016/j.juro.2015.11.029. ISSN 1527-3792. PMC 5609078. PMID 26901507.
- ^ "Kidney Cancer Stages | Renal Cell Carcinoma Staging". www.cancer.org. Retrieved 2019-11-12.
- ^ أ ب ت ث ج ح خ AJCC cancer staging manual. Edge, Stephen B., American Joint Committee on Cancer. (7th ed. ed.). New York: Springer. 2010. ISBN 9780387884400. OCLC 316431417.
{{cite book}}:|edition=has extra text (help)CS1 maint: others (link) - ^ أ ب "Kidney Cancer (Adult) – Renal Cell Carcinoma" (PDF). American Cancer Society. Archived from the original (PDF) on 2017-02-22. Last Revised: May 16, 2016
- ^ Motzer, Robert J.; Jonasch, Eric; Agarwal, Neeraj; Bhayani, Sam; Bro, William P.; Chang, Sam S.; Choueiri, Toni K.; Costello, Brian A.; Derweesh, Ithaar H.; Fishman, Mayer; Gallagher, Thomas H. (2017-06-01). "Kidney Cancer, Version 2.2017, NCCN Clinical Practice Guidelines in Oncology". Journal of the National Comprehensive Cancer Network. 15 (6): 804–834. doi:10.6004/jnccn.2017.0100. ISSN 1540-1405.
- ^ "Early stage and locally advanced kidney cancer treatment". 2017-08-30.
- ^ "Advanced kidney cancer". 2017-08-30.
- ^ "Renal cancer".
- ^ "National Comprehensive Cancer Network" (PDF).
- ^ "Biological therapy for kidney cancer". 2017-08-30.
- ^ Jonasch, Eric; Messner, Carolyn (August 2012). "CancerCare Connect – Treatment Update: Kidney Cancer" (PDF). Cancer Care, Inc. Archived from the original (PDF) on 2011-09-25. Retrieved 2012-08-29.
- ^ أ ب Syn, Nicholas L; Teng, Michele W L; Mok, Tony S K; Soo, Ross A (2017). "De-novo and acquired resistance to immune checkpoint targeting". The Lancet Oncology. 18 (12): e731–e741. doi:10.1016/s1470-2045(17)30607-1. PMID 29208439.
- ^ "FDA approves Opdivo to treat advanced form of kidney cancer".
- ^ Philips, GK; Atkins, MB (2014). "New agents and new targets for renal cell carcinoma". American Society of Clinical Oncology Educational Book / ASCO. American Society of Clinical Oncology. Meeting. 34: e222-7. doi:10.14694/EdBook_AM.2014.34.e222. PMID 24857106.
- ^ "Drugs@FDA: FDA Approved Drug Products".
- ^ http://www.accessdata.fda.gov/drugsatfda_docs/label/2016/208692s000lbl.pdf
- ^ http://www.accessdata.fda.gov/drugsatfda_docs/label/2015/206947s000lbl.pdf
- ^ أ ب "Wilms' tumour (kidney cancer in children)". 2017-08-30. Archived from the original on 2012-04-06.
- ^ Lindblad, P. and Adami H.O, Kidney Cancer, in Textbook of Cancer.
- ^ GLOBOCAN 2002, Cancer Incidence, Mortality and Prevalence Worldwide 2002 estimates. 2006.
- ^ "Kidney Cancer". National Cancer Institute, U.S. National Institutes of Health. Retrieved 2009-03-03.
- ^ Coleman JA (2008). "Familial and hereditary renal cancer syndromes". Urol. Clin. North Am. 35 (4): 563–72, v. doi:10.1016/j.ucl.2008.07.014. PMID 18992610.
{{cite journal}}: Unknown parameter|month=ignored (help)