سعات الرئة
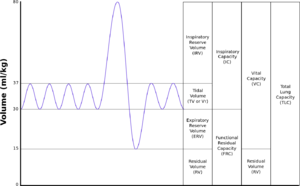
| TLC | السعة الإجمالية للرئة: الحجم في الرئتين عند أقصى تدفق، مجموع VC وRV. |
|---|---|
| TV | حجم المدى: حجم الهواء الداخل والخارج من الرئتين أثناء التنفس الهادئ (يشير TV إلى تقسيم الرئة؛ عند قياس حجم المدى بدقة، يستخدم الرمز TV أو VT كما في حساب تبادل الغازات.) |
| RV | الحجم المتبقي: حجم الهواء المتبقي في الرئتين بعد أقصى زفير. |
| ERV | حجم الاحتياطي الزفيري: الحجم الأقصى من الهواء الذي يمكن زفيره من وضع الزفير النهائي. |
| IRV | حجم الاحتياطي الشهيقي: الحجم الأقصى من الهواء الذي يمكن شهيقه من مستوى الشهيق النهائي. |
| IC | السعة الشهيقية: مجمو IRV وTV |
| IVC | السعة الحيوية الشهيقية: الحجم الأقصى من الهواء الذي يستنشق من نقطة الزفير القصوى. |
| VC | السعة الحيوية: حجم الهواء الخارج بعد أعمق استنشاق. |
| VT | ججم المدى: حجم الهواء الداخل والخارج من الرئتين أثناء التنفس الهادئ (يشير VT إلى تقسيم الرئة؛ عند قياس حجم المدى بدقة، يستخدم الرمز TV أو VT كما في حساب تبادل الغازات.) |
| FRC | السعة المتبقية الوظيفية: الحجم في الرئتين عند وضع الزفير النهائي. |
| RV/TLC% | يعبر الحجم المتبقي عن النسبة المئوية لـ TLC |
| VA | حجم الغاز السنخي |
| VL | الحجم الحقيقي للرئة ويشمل حجم الشعب الهوائية الموصلة. |
| FVC | السعة الحيوية القسرية: تحديد السعة الحيوية من عملية الزفير القسري الأقصى. |
| FEVt | الحجم الزفيري القسري (الزمن): مصطلح عام يشير إلى حجم الهواء الخارج تحت ظروف قسرية في أول t ثواني |
| FEV1 | حجم الهواء الخارج عند نهاية الثانية الأولى من الزفير القسري. |
| FEFx | يرتبط تدفق الزفير القسري ببعض مناطق منحنى FVC؛ تشير التعديلات إلى كمية FVC الخارجة بالفعل |
| FEFmax | الحد الأقصى للتدفق الفوري أثناء إجراء FVC |
| FIF | تدفق الزفير القسري: (قياس محدد لمنحنى التنفس القسري مشار إليه بتسميات مشابهة لتلك المستخدمة في منحنى الزفير القسري. على سبيل المثال، يشار إلى تدفق التنفس الأقصى بالرمز FIFmax. ما لم يحدد غير ذلك، فإن معدلات الحجم تشير إلى حجم الزفير من RV عند نقطة القياس.) |
| PEF | ذروة التدفق الزفيري: أعلى تدفق زفيري قسري على ذروة مقياس التدفق. |
| MVV | التنفس الطوعي الأقصى: حجم الهواء الخارج من الرئتين في فترة محددة أثناء التنفس الاقصى المتكرر |
Lung volumes and lung capacities refer to the volume of air in the lungs at different phases of the respiratory cycle.
The average total lung capacity of an adult human male is about 6 litres of air.
Tidal breathing is normal, resting breathing; the tidal volume is the volume of air that is inhaled or exhaled in only a single such breath.
The average human respiratory rate is 30–60 breaths per minute at birth,[1] decreasing to 12–20 breaths per minute in adults.[2]
Factors affecting volumes
Several factors affect lung volumes; some can be controlled, and some cannot be controlled. Lung volumes vary with different people as follows:
| Larger volume | Smaller volumes |
|---|---|
| taller people | shorter people |
| people who live at higher altitudes | people who live at lower altitudes |
| fit | obese[3] |
A person who is born and lives at sea level will develop a slightly smaller lung capacity than a person who spends their life at a high altitude. This is because the partial pressure of oxygen is lower at higher altitude which, as a result means that oxygen less readily diffuses into the bloodstream. In response to higher altitude, the body's diffusing capacity increases in order to process more air. Also, due to the lower environmental air pressure at higher altitudes, the air pressure within the breathing system must be lower in order to inhale; in order to meet this requirement, the thoracic diaphragm has a tendency to lower to a greater extent during inhalation, which in turn causes an increase in lung volume.
When someone living at or near sea level travels to locations at high altitudes (e.g. the Andes; Denver, Colorado; Tibet; the Himalayas) that person can develop a condition called altitude sickness because their lungs remove adequate amounts of carbon dioxide but they do not take in enough oxygen. (In normal individuals, carbon dioxide is the primary determinant of respiratory drive.)
Lung function development is reduced in children who grow up near motorways[4][5] although this seems at least in part reversible.[6] Air pollution exposure affects FEV1 in asthmatics, but also affects FVC and FEV1 in healthy adults even at low concentrations.[7]
Specific changes in lung volumes also occur during pregnancy. Functional residual capacity drops 18–20%,[8] typically falling from 1.7 to 1.35 litres,[citation needed] due to the compression of the diaphragm by the uterus.[citation needed] The compression also causes a decreased total lung capacity (TLC) by 5%[8] and decreased expiratory reserve volume by 20%.[8] Tidal volume increases by 30–40%, from 0.5 to 0.7 litres,[8] and minute ventilation by 30–40%[8][9] giving an increase in pulmonary ventilation. This is necessary to meet the increased oxygen requirement of the body, which reaches 50 ml/min, 20 ml of which goes to reproductive tissues. Overall, the net change in maximum breathing capacity is zero.[8]
Values
| Volume | Value (litres) | |
|---|---|---|
| In men | In women | |
| Inspiratory reserve volume (IRV) | 3.3 | 1.9 |
| Tidal volume (TV) | 0.5 | 0.5 |
| Expiratory reserve volume (ERV) | 1.1 | 0.7 |
| Residual volume (RV) | 1.2 | 1.1 |
| Volume | Average value (litres) | Derivation | |
|---|---|---|---|
| In men | In women | ||
| Vital capacity | 4.8 | 3.1 | IRV + TV + ERV |
| Inspiratory capacity | 3.8 | 2.4 | IRV + TV |
| Functional residual capacity | 2.4 | 1.8 | ERV + RV |
| Total lung capacity | 6.0 | 4.2 | IRV + TV + ERV + RV |
The tidal volume, vital capacity, inspiratory capacity and expiratory reserve volume can be measured directly with a spirometer. These are the basic elements of a ventilatory pulmonary function test.
Determination of the residual volume is more difficult as it is impossible to "completely" breathe out. Therefore, measurement of the residual volume has to be done via indirect methods such as radiographic planimetry, body plethysmography, closed circuit dilution (including the helium dilution technique) and nitrogen washout.
In absence of such, estimates of residual volume have been prepared as a proportion of body mass for infants (18.1 ml/kg),[11] or as a proportion of vital capacity (0.24 for men and 0.28 for women)[12] or in relation to height and age ((0.0275* Age [Years]+0.0189*Height [cm]−2.6139) litres for normal-mass individuals and (0.0277*Age [Years]+0.0138*Height [cm]−2.3967) litres for overweight individuals).[13] Standard errors in prediction equations for residual volume have been measured at 579 ml for men and 355 ml for women, while the use of 0.24*FVC gave a standard error of 318 ml.[14]
Online calculators are available that can compute predicted lung volumes, and other spirometric parameters based on a patient's age, height, weight, and ethnic origin for many reference sources.
British rower and three-time Olympic gold medalist, Pete Reed, is reported to hold the largest recorded lung capacity of 11.68 litres;[15][16][17] US swimmer, Michael Phelps is also said to have a lung capacity of around 12 litres.[16][18]
Weight of breath
The mass of one breath is approximately a gram (0.5-5 g). A litre of air weighs about 1.2 g (1.2 kg/m3).[19] A half litre ordinary tidal breath[10] weighs 0.6 g; a maximal 4.8 litre breath (average vital capacity for males)[10] weighs approximately 5.8 g.
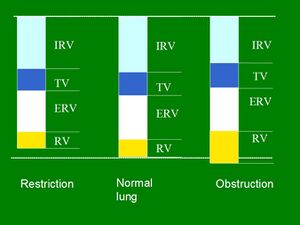
Restrictive and obstructive
The results (in particular FEV1/FVC and FRC) can be used to distinguish between restrictive and obstructive pulmonary diseases:
| Type | Examples | Description | FEV1/FVC |
| restrictive diseases | pulmonary fibrosis, Infant Respiratory Distress Syndrome, weak respiratory muscles, pneumothorax | volumes are decreased | often in a normal range (0.8–1.0) |
| obstructive diseases | asthma, COPD, emphysema | volumes are essentially normal but flow rates are impeded | often low (asthma can reduce the ratio to 0.6, emphysema can reduce the ratio to 0.78–0.45) |
انظر أيضاً
المراجع
- ^ Scott L. DeBoer (4 November 2004). Emergency Newborn Care. Trafford Publishing. p. 30. ISBN 978-1-4120-3089-2.
- ^ Wilburta Q. Lindh; Marilyn Pooler; Carol Tamparo; Barbara M. Dahl (9 March 2009). Delmar's Comprehensive Medical Assisting: Administrative and Clinical Competencies. Cengage Learning. p. 573. ISBN 978-1-4354-1914-8.
- ^ Jones RL, Nzekwu MM (2006). "The effects of body mass index on lung volumes". Chest. 130 (3): 827–33. doi:10.1378/chest.130.3.827. PMID 16963682.
- ^ Living Near Freeways Hurts Kids' Lungs https://www.washingtonpost.com/wp-dyn/content/article/2007/01/26/AR2007012600568.html
- ^ Gauderman, W (2007). "Effect of exposure to traffic on lung development from 10 to 18 years of age: a cohort study". The Lancet. 369 (9561): 571–577. CiteSeerX 10.1.1.541.1258. doi:10.1016/S0140-6736(07)60037-3. PMID 17307103. S2CID 852646.
- ^ "Study Findings – USC Children's Health Study".
- ^ Int Panis, L (2017). "Short-term air pollution exposure decreases lung function: a repeated measures study in healthy adults". Environmental Health. 16 (1): 60. doi:10.1186/s12940-017-0271-z. PMC 5471732. PMID 28615020.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ أ ب ت ث ج ح Simpson, Kathleen Rice; Patricia A Creehan (2007). Perinatal Nursing (3rd ed.). Lippincott Williams & Wilkins. pp. 65–66. ISBN 978-0-7817-6759-0.
- ^ Guyton and hall (2005). Textbook of Medical Physiology (11 ed.). Philadelphia: Saunders. pp. 103g. ISBN 978-81-8147-920-4.
- ^ أ ب ت ث Tortora, Gerard J. (2016). Principles of anatomy & physiology. Derrickson, Bryan (15th ed.). Hoboken, NJ. p. 874. ISBN 978-1119447979. OCLC 1020568457.
{{cite book}}: CS1 maint: location missing publisher (link) - ^ Morris, Mohy G. (2010). "Comprehensive integrated spirometry using raised volume passive and forced expirations and multiple-breath nitrogen washout in infants". Respiratory Physiology & Neurobiology. 170 (2): 123–140. doi:10.1016/j.resp.2009.10.010. ISSN 1569-9048. PMC 2858579. PMID 19897058.
- ^ Wilmore, J. H. (1969). "The use of actual predicted and constant residual volumes in the assessment of body composition by underwater weighing". Med Sci Sports. 1 (2): 87–90. doi:10.1249/00005768-196906000-00006.
- ^ MILLER, WAYNE C.; SWENSEN, THOMAS; WALLACE, JANET P. (February 1998). "Derivation of prediction equations for RV in overweight men and women". Medicine & Science in Sports & Exercise. 30 (2): 322–327. doi:10.1097/00005768-199802000-00023. PMID 9502364.
- ^ Morrow JR Jr; Jackson AS; Bradley PW; Hartung GH. (Dec 1986). "Accuracy of measured and predicted residual lung volume on body density measurement". Med Sci Sports Exerc. 18 (6): 647–52. doi:10.1249/00005768-198612000-00007. PMID 3784877.
- ^ English Institute of Sport, 17 November 2006, test ID 27781
- ^ أ ب "Making sense of breathing, VO2max and lung capacity". worldrowing.com (in الإنجليزية الأمريكية). Retrieved 2019-11-28.
- ^ "Pete Reed: Three-time Olympic rowing champion on spinal stroke, paralysis and the future" (in الإنجليزية البريطانية). 2019-11-28. Retrieved 2019-11-28.
- ^ Smith, Michael Hanlon and Jennifer (2012-08-03). "London 2012 Olympics: Faster. Higher. Longer. Stronger". Daily Telegraph (in الإنجليزية البريطانية). ISSN 0307-1235. Retrieved 2019-11-28.
- ^ Atmosphere of Earth#Density and mass
وصلات خارجية
- CS1 maint: unflagged free DOI
- CS1 maint: location missing publisher
- CS1 الإنجليزية الأمريكية-language sources (en-us)
- CS1 الإنجليزية البريطانية-language sources (en-gb)
- Short description matches Wikidata
- Articles with unsourced statements from January 2010
- Articles with unsourced statements from October 2013
- Respiratory physiology
- Pulmonary function testing