كوراري
الكوراري (إنگليزية: Curare؛ أصد: [k(j)uːˈrɑːri] [1]) مستخرج نباتي سام من بعض نباتات أمريكا الجنوبية وخاصة من نوع كونرودندرون وسترايكنوز. تستخدم مشتقات الكورار طبيًا لإحداث الاسترخاء العضلي في أثناء العمليات الجراحية كما يستخدم للمرضى المحتاجين للتهوية الآلية.
التاريخ
وكان هنود أمريكا الجنوبية يستخدمون السهام المسممة بالكورار في الصيد مئات السنين. وعندما يدخل السم مجرى دم الحيوان أو أنسجته، يسبب شللاً للعضلات، بما في ذلك العضلات الضرورية للتنفس، فيموت الحيوان اختناقًا.
في 1596 ذكر السير والتر رالي سم السهم في كتابه Discovery of the Large, Rich, and Beautiful Empire of Guiana (وهي گويانا الحالية)، بالرغم من أنه من الممكن أن السم الذي وصفه لم يكن كوراري على الإطلاق.[2] وفي 1780، اكتشف الأب فليكس فونتانا أنه يعمل على قدرة الأعصاب اللا إرادية بدلاً من العمل على الأعصاب والقلب.[3] وفي 1800، أعطى ألكسندر فون هومبولت أول وصف اوروبي غربي لكيفية تحضير السم من النبات من قِبل سكان نهر اورينوكو.[4]
أثناء 1811-1812 أجرى السير بنجامين كولنز برودي (1783-1862) تجارب على الكوراري.[5] He was the first to show that curare does not kill the animal and the recovery is complete if the animal’s respiration is maintained artificially. وفي 1825 وصف تشارلز واترتون تجربة كلاسيكية احتفظ فيها بأنثى حمار تناولت الكوراري حية بواسطة التنفس الصناعي بنفاخات موصلة بثقب في القصبة الهوائية.[6] Waterton is also credited with bringing curare to Europe.[7] روبرت هرمان شومبورك, who was a trained botanist, identified the vine as one of the Strychnos genus and gave it the now accepted name Strychnos toxifera.[8]
وفي عام 1856م، أوضح عالم وظائف الأعضاء الفرنسي كلود برنارد، أن الكورار يمنع وصول النبضات العصبية إلى العضلة الإرادية. وفي النصف الثاني من القرن التاسع عشر الميلادي استخدم بعض الأطباء الكورار في معالجة الصرع والكزاز.
الخصائص الصيدلية
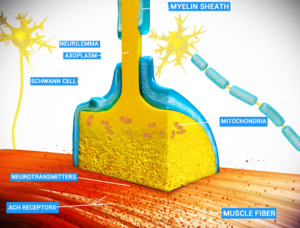
Curare is an example of a non-depolarizing muscle relaxant that blocks the nicotinic acetylcholine receptor (nAChR),[9] one of the two types of acetylcholine (ACh) receptors, at the neuromuscular junction. The main toxin of curare, d-tubocurarine, occupies the same position on the receptor as ACh with an equal or greater affinity, and elicits no response, making it a competitive antagonist. The antidote for curare poisoning is an acetylcholinesterase (AChE) inhibitor (anti-cholinesterase), such as physostigmine or neostigmine. By blocking ACh degradation, AChE inhibitors raise the amount of ACh in the neuromuscular junction; the accumulated ACh will then correct for the effect of the curare by activating the receptors not blocked by toxin at a higher rate.
The time of onset varies from within one minute (for tubocurarine in intravenous administration, penetrating a larger vein), to between 15 and 25 minutes (for intramuscular administration, where the substance is applied in muscle tissue).[9]
It is harmless if taken orally[10][11] because curare compounds are too large and highly charged to pass through the lining of the digestive tract to be absorbed into the blood. For this reason, people can safely eat curare-poisoned prey, and it has no effect on its flavor.[12]
التخدير
Isolated attempts to use curare during anesthesia date back to 1912 by Arthur Lawen of Leipzig,[13] but curare came to anesthesia via psychiatry (electroplexy). In 1939 Abram Elting Bennett used it to modify metrazol induced convulsive therapy.[14] Muscle relaxants are used in modern anesthesia for many reasons, such as providing optimal operating conditions and facilitating intubation of the trachea. Before muscle relaxants, anesthesiologists needed to use larger doses of the anesthetic agent, such as ether, chloroform or cyclopropane to achieve these aims. Such deep anesthesia risked killing patients who were elderly or had heart conditions.
The source of curare in the Amazon was first researched by Richard Evans Schultes in 1941. Since the 1930s, it was being used in hospitals as a muscle relaxant. He discovered that different types of curare called for as many as 15 ingredients, and in time helped to identify more than 70 species that produced the drug.
In the 1940s, it was used on a few occasions during surgery as it was mistakenly thought to be an analgesic or anesthetic. The patients reported feeling the full intensity of the pain though they were not able to do anything about it since they were essentially paralyzed.[15]
On January 23, 1942, Harold Griffith and Enid Johnson gave a synthetic preparation of curare (Intercostrin/Intocostrin) to a patient undergoing an appendectomy (to supplement conventional anesthesia). Safer curare derivatives, such as rocuronium and pancuronium, have superseded d-tubocurarine for anesthesia during surgery. When used with halothane d-tubocurarine can cause a profound fall in blood pressure in some patients as both the drugs are ganglion blockers.[16] However, it is safer to use d-tubocurarine with ether.
In 1954, an article was published by Beecher and Todd suggesting that the use of muscle relaxants (drugs similar to curare) increased death due to anesthesia nearly sixfold.[17] This was refuted in 1956.[18]
Modern anesthetists have at their disposal a variety of muscle relaxants for use in anesthesia. The ability to produce muscle relaxation irrespective of sedation has permitted anesthetists to adjust the two effects independently and on the fly to ensure that their patients are safely unconscious and sufficiently relaxed to permit surgery. The use of neuromuscular blocking drugs carries with it the risk of anesthesia awareness.
الهامش
- ^ curare - definition of curare by the Free Online Dictionary, Thesaurus and Encyclopedia
- ^ Carman J. A. Anaesthesia 1968, 23, 706.
- ^ The Gale Encyclopedia of Science. Third Edition.
- ^ [1]Personal Narrative of Travels to the Equinoctial Regions of America, During the Year 1799-1804 — Volume 2, Humboldt, Alexander von
- ^ Phil. Trans. 1811, 101, 194; 1812, 102, 205.
- ^ Arrow Poison to Surgical Muscle Relaxant
- ^ Reprinted in "Classical File", Survey of Anesthesiology 1978, 22, 98.
- ^ and Wouralia. British Journal of Pharmacology (1999) 126, 1685–1689
- ^ أ ب "Curare". Drugs.com. 8 November 2001. Archived from the original on 16 November 2018. Retrieved 23 January 2018.
- ^ "Curare (Chondrodendron tomentosum - Menispermaceae): From Arrow Poison to Surgical Muscle Relaxant". Ye Olde Log. n.d. Archived from the original on 9 May 2008. Retrieved 23 August 2017.
- ^ Schaffner, Brynn (2000). "Curare". Blue Planet Biomes. Retrieved 14 April 2020.
- ^ Milner, Daniel (Summer 2009). "From the Rainforests of South America to The Operating Room: A History of Curare". Faculty of Medicine, Department of Innovation in Medical Education. University of Ottawa. Archived from the original on 30 July 2011.
- ^ Lawen, A. (1912). "Über die Verbindung der Lokalanästhesie mit der Narkose, über hohe Extraduralanaesthesie und epidurale injektionen anasthesierender Losungen bei tabischen Makenkrisen" [Over the connection of local anesthesia with anesthesia, through high extradural anesthesia and epidural injections of anesthetic solutions in tabetic macaques]. Beiträge zur klinischen Chirurgie (in الألمانية). 80: 168–189.
- ^ Bennett, A. E. (1940). "Preventing traumatic complications in convulsive shock therapy by curare". Journal of the American Medical Association. American Medical Association. 114 (4): 322–324. doi:10.1001/jama.1940.02810040032009.
- ^ Dennett, Daniel C. (1978). Brainstorms: Philosophical Essays on Mind and Psychology. Cambridge, Massachusetts: The MIT Press. p. 209.
- ^ Mashraqui, S. (October 1994). "Hypotension induced with d-tubocurarine and halothane for surgery of patent ductus arteriosus". Indian Journal of Anaesthesia. 42 (5): 346–50.
- ^ Beecher, H. K.; Todd, D. P. (1954). "A Study of the Deaths Associated with Anesthesia and Surgery: Based on a Study of 599,548 Anesthesias in Ten Institutions 1948–1952, Inclusive". Annals of Surgery. 140 (2): 2–35. doi:10.1097/00000658-195407000-00001. PMC 1609600. PMID 13159140., reprinted in "Classical File". Survey of Anesthesiology. 15 (5): 496 ff. October 1971. doi:10.1097/00132586-197110000-00013.
- ^ Albertson, HA; Trout, HH; Morfin, E (June 1956). "The Safety of Curare in Anesthesia". Annals of Surgery. 143 (6): 833–837. doi:10.1097/00000658-195606000-00012. PMC 1465152. PMID 13327828.
المصادر
- Foldes, F.F. "Anesthesia before and after curare", Anasthesieabteilung des Albert-Einstein-College of Medicine. Anaesthesiol Reanim, 1993, 18(5):128-31. (retrieved June 20 2005)
- James, Mel. "Harold Griffith",Heirloom Series, Volume 6. (retrieved June 20 2005)
- "Curare", Blue Planet Biomes, 2000. (retrieved September 27 2005)
- Smith, Roger. "Cholernergic Transmission", (retrieved March 13, 2007)
- Strecker G J et al. "Curare binding and the curare-induced subconductance state of the acetylcholine receptor channel.", Biophysical Journal 56: 795-806 (1989). (retrieved May 12, 2007)
