القنب الطبي
| جزء من سلسلة عن |
| القنب |
|---|
 |
Medical cannabis, or medical marijuana (MMJ), is cannabis and cannabinoids that are prescribed by physicians for their patients.[1][2] The use of cannabis as medicine has not been rigorously tested due to production and governmental restrictions, resulting in limited clinical research to define the safety and efficacy of using cannabis to treat diseases.[3] Preliminary evidence suggests that cannabis can reduce nausea and vomiting during chemotherapy, improve appetite in people with HIV/AIDS, reduces chronic pain and muscle spasms[4][5][6] and treats severe forms of epilepsy.[7]
Short-term use increases the risk of minor and major adverse effects.[5] Common side effects include dizziness, feeling tired, vomiting, and hallucinations.[5] Long-term effects of cannabis are not clear.[5] Concerns include memory and cognition problems, risk of addiction, schizophrenia in young people, and the risk of children taking it by accident.[4]
The Cannabis plant has a history of medicinal use dating back thousands of years in many cultures.[8] Some American medical organizations have requested removal of cannabis from the list of Schedule I controlled substances maintained by the United States federal government, followed by regulatory and scientific review.[9][10] Others oppose its legalization, such as the American Academy of Pediatrics.[11]
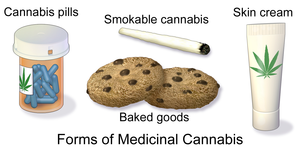
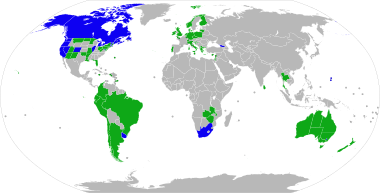
Medical cannabis can be administered through various methods, including capsules, lozenges, tinctures, dermal patches, oral or dermal sprays, cannabis edibles, and vaporizing or smoking dried buds. Synthetic cannabinoids are available for prescription use in some countries, such as dronabinol and nabilone. Countries that allow the medical use of whole-plant cannabis include Australia, Canada, Chile, Colombia, Germany, Greece, Israel, Italy, the Netherlands, Peru, Poland, Portugal, and Uruguay. In the United States, 33 states and the District of Columbia have legalized cannabis for medical purposes, beginning with the passage of California's Proposition 215 in 1996.[12] Although cannabis remains prohibited for any use at the federal level, the Rohrabacher–Farr amendment was enacted in December 2014, limiting the ability of federal law to be enforced in states where medical cannabis has been legalized.
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
Classification
The National Institute on Drug Abuse defines medical cannabis as "using the whole, unprocessed marijuana plant or its basic extracts to treat symptoms of illness and other conditions".[13]
A Cannabis plant includes more than 400 different chemicals, of which about 70 are cannabinoids.[14] In comparison, typical government-approved medications contain only one or two chemicals.[14] The number of active chemicals in cannabis is one reason why treatment with cannabis is difficult to classify and study.[14]
A 2014 review stated that the variations in ratio of CBD-to-THC in botanical and pharmaceutical preparations determines the therapeutic vs psychoactive effects (CBD attenuates THC's psychoactive effects[15]) of cannabis products.[16]
الاستخدامات الطبية
It is not clear whether medical cannabis is a useful treatment for any condition.[5] Evidence is moderate that it helps in chronic pain and muscle spasms.[5] Low quality evidence suggests its use for reducing nausea during chemotherapy, improving appetite in HIV/AIDS, improving sleep, and improving tics in Tourette syndrome.[5] When usual treatments are ineffective, cannabinoids have also been recommended for anorexia, arthritis, glaucoma,[17] and migraine.[18] It is unclear whether American states might be able to mitigate the adverse effects of the opioid epidemic by prescribing medical cannabis as an alternative pain management drug.[19]
It is recommended that cannabis use be stopped in pregnancy.[20]
الغثيان والقيء
Medical cannabis is somewhat effective in chemotherapy-induced nausea and vomiting (CINV)[4][17] and may be a reasonable option in those who do not improve following preferential treatment.[21] Comparative studies have found cannabinoids to be more effective than some conventional antiemetics such as prochlorperazine, promethazine, and metoclopramide in controlling CINV,[22] but these are used less frequently because of side effects including dizziness, dysphoria, and hallucinations.[23][24] Long-term cannabis use may cause nausea and vomiting, a condition known as cannabinoid hyperemesis syndrome (CHS).[25]
A 2016 Cochrane review said that cannabinoids were "probably effective" in treating chemotherapy-induced nausea in children, but with a high side-effect profile (mainly drowsiness, dizziness, altered moods, and increased appetite). Less common side effects were "ocular problems, orthostatic hypotension, muscle twitching, pruritus, vagueness, hallucinations, lightheadedness and dry mouth".[26]
الإيدز
Evidence is lacking for both efficacy and safety of cannabis and cannabinoids in treating patients with HIV/AIDS or for anorexia associated with AIDS. As of 2013, current studies suffer from the effects of bias, small sample size, and lack of long-term data.[27]
الألم
A 2017 review found only limited evidence for the effectiveness of cannabis in relieving chronic pain in several conditions.[28] Another review found tentative evidence for use of cannabis in treating peripheral neuropathy, but little evidence of benefit for other types of long term pain.[29]
When cannabis is inhaled to relieve pain, blood levels of cannabinoids rise faster than when oral products are used, peaking within three minutes and attaining an analgesic effect in seven minutes.[28] A 2014 review found limited and weak evidence that smoked cannabis was effective for chronic non-cancer pain.[30] A 2015 meta-analysis found that inhaled medical cannabis was effective in reducing neuropathic pain in the short term for one in five to six patients.[31] Another 2015 review found limited evidence that medical cannabis was effective for neuropathic pain when combined with traditional analgesics.[32]
A 2011 review considered cannabis to be generally safe,[33] and it appears safer than opioids in palliative care.[34]
الأحوال العصبية
Cannabis' efficacy is not clear in treating neurological problems, including multiple sclerosis (MS) and movement problems.[16] The combination of Δ9-tetrahydrocannabinol (THC) and cannabidiol (CBD) extracts give subjective relief of spasticity, though objective post-treatment assessments do not reveal significant changes.[35] Evidence also suggests that oral cannabis extract is effective for reducing patient-centered measures of spasticity.[16] A trial of cannabis is deemed to be a reasonable option if other treatments have not been effective.[4][ممن؟] Its use for MS is approved in ten countries.[4][36]قالب:COI source A 2012 review found no problems with tolerance, abuse, or addiction.[37] In the United States, cannabidiol, one of the cannabinoids found in the marijuana plant, has been approved for treating two severe forms of epilepsy, Lennox-Gastaut syndrome and Dravet syndrome.[7]
اضطراب ضغوط ما بعد الحوادث
There is no good evidence that medical cannabis is effective for treating posttraumatic stress disorder, and its use for this purpose is not recommended.[38]
الآثار الجانبية
الاستخدام الطبي
There is insufficient data to draw strong conclusions about the safety of medical cannabis.[39] Typically, adverse effects of medical cannabis use are not serious;[4] they include tiredness, dizziness, increased appetite, and cardiovascular and psychoactive effects. Other effects can include impaired short-term memory; impaired motor coordination; altered judgment; and paranoia or psychosis at high doses.[40] Tolerance to these effects develops over a period of days or weeks. The amount of cannabis normally used for medicinal purposes is not believed to cause any permanent cognitive impairment in adults, though long-term treatment in adolescents should be weighed carefully as they are more susceptible to these impairments. Withdrawal symptoms are rarely a problem with controlled medical administration of cannabinoids. The ability to drive vehicles or to operate machinery may be impaired until a tolerance is developed.[21] Although supporters of medical cannabis say that it is safe,[39] further research is required to assess the long-term safety of its use.[23][41]
الاستخدام الترفيهي
Tetrahydrocannabinol (THC), the principal psychoactive constituent of the cannabis plant, has low toxicity while the LD50 (dose of THC needed to kill 50% of tested rodents) is high. Acute effects may include anxiety and panic, impaired attention, and memory (while intoxicated), an increased risk of psychotic symptoms, and possibly increased risk of accidents if a person drives a motor vehicle while intoxicated.[42] Psychotic episodes are well-documented and typically resolve within minutes or hours. There have been few reports of symptoms lasting longer.[43][44]
According to the United States Department of Health and Human Services, there were 455,000 emergency room visits associated with cannabis use in 2011. These statistics include visits in which the patient was treated for a condition induced by or related to recent cannabis use. The drug use must be "implicated" in the emergency department visit, but does not need to be the direct cause of the visit. Most of the illicit drug emergency room visits involved multiple drugs.[45] In 129,000 cases, cannabis was the only implicated drug.[46][47]
Effects of chronic use may include bronchitis, a cannabis dependence syndrome, and subtle impairments of attention and memory. These deficits persist while chronically intoxicated.[42] Compared to non-smokers, people who smoked cannabis regularly in adolescence exhibit reduced connectivity in specific brain regions associated with memory, learning, alertness, and executive function.[47] One study suggested that sustained heavy, daily, adolescent onset cannabis use over decades is associated with a decline in IQ by age 38, with no effects found in those who initiated cannabis use later, or in those who ceased use earlier in adulthood.[48] A follow-up review found that IQ deficit may be a precursor, rather than result, of cannabis use, and that social and environmental factors are a likely influence.[49]
There has been a limited amount of studies that have looked at the effects of smoking cannabis on the respiratory system.[50] Chronic heavy marijuana smoking is associated with coughing, production of sputum, wheezing, coughing, and other symptoms of chronic bronchitis.[42] Regular cannabis use has not been shown to cause significant abnormalities in lung function.[51]
Cannabis smoke contains thousands of organic and inorganic chemical compounds. This tar is chemically similar to that found in tobacco smoke,[52] and over fifty known carcinogens have been identified in cannabis smoke,[53] including nitrosamines, reactive aldehydes, and polycyclic hydrocarbons, including benz[a]pyrene.[54] Light and moderate use of cannabis is not believed to increase risk of lung or upper airway cancer. Evidence for causing these cancers is mixed concerning heavy, long-term use. In general there are far lower risks of pulmonary complications for regular cannabis smokers when compared with those of tobacco.[51] Combustion products are not present when using a vaporizer, consuming THC in pill form, or consuming cannabis edibles.
There is serious suspicion among cardiologists, spurring research but falling short of definitive proof, that cannabis use has the potential to contribute to cardiovascular disease.[55] Cannabis is believed to be an aggravating factor in rare cases of arteritis, a serious condition that in some cases leads to amputation. Because 97% of case-reports also smoked tobacco, a formal association with cannabis could not be made. If cannabis arteritis turns out to be a distinct clinical entity, it might be the consequence of vasoconstrictor activity observed from delta-8-THC and delta-9-THC.[56] Other serious cardiovascular events including myocardial infarction, stroke, sudden cardiac death, and cardiomyopathy have been reported to be temporally associated with cannabis use. Research in these events is complicated because cannabis is often used in conjunction with tobacco, and drugs such as alcohol and cocaine.[57] These putative effects can be taken in context of a wide range of cardiovascular phenomena regulated by the endocannabinoid system and an overall role of cannabis in causing decreased peripheral resistance and increased cardiac output, which potentially could pose a threat to those with cardiovascular disease.[58]
Cannabis usually causes no tolerance or withdrawal symptoms except in heavy users. In a survey of heavy users 42.4% experienced withdrawal symptoms when they tried to quit marijuana such as craving, irritability, boredom, anxiety and sleep disturbances.[59] About 9% of those who experiment with marijuana eventually become dependent. The rate goes up to one in six among those who begin use as adolescents, and one-quarter to one-half of those who use it daily according to a NIDA review.[47] A 2013 review estimates daily use is associated with a 10-20% rate of dependence.[4] The highest risk of cannabis dependence is found in those with a history of poor academic achievement, deviant behavior in childhood and adolescence, rebelliousness, poor parental relationships, or a parental history of drug and alcohol problems.[60]
A 2013 literature review found that exposure to marijuana had biologically-based physical, mental, behavioral and social health consequences and was "associated with diseases of the liver (particularly with co-existing hepatitis C), lungs, heart, and vasculature".[61] There are numerous other reasons why people look for medical cannabis and to make people aware of whether they are eligible to accept medical cannabis as a dose, there are numerous websites that are currently providing online consultations through video calling. People are provided licenses with the help of which, they can either grow medical cannabis, or purchase it legally throughout the state. This is done only after precisely reviewing the applications of patients.[62]
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
Cognitive effects
A 2011 systematic review evaluated published studies of the acute and long-term cognitive effects of cannabis. THC intoxication is well established to impair cognitive functioning on an acute basis, including effects on the ability to plan, organize, solve problems, make decisions, and control impulses. The extent of this impact may be greater in novice users, and paradoxically, those habituated to high-level ingestion may have reduced cognition during withdrawal. Studies of long-term effects on cognition have provided conflicting results, with some studies finding no difference between long-term abstainers and never-users and others finding long-term deficits. The discrepancies between studies may reflect greater long-term effects among heavier users relative to occasional users, and greater duration of effect among those with heavy use as adolescents compared to later in life.[63] A second systematic review focused on neuroimaging studies found little evidence supporting an effect of cannabis use on brain structure and function.[64] A 2003 meta-analysis concluded that any long-term cognitive effects were relatively modest in magnitude and limited to certain aspects of learning and memory.[65]
Impact on psychosis
Exposure to THC can cause acute transient psychotic symptoms in healthy individuals and people with schizophrenia.[15]
A 2007 meta analysis concluded that cannabis use reduced the average age of onset of psychosis by 2.7 years relative to non-cannabis use.[66] A 2005 meta analysis concluded that adolescent use of cannabis increases the risk of psychosis, and that the risk is dose-related.[67] A 2004 literature review on the subject concluded that cannabis use is associated with a two-fold increase in the risk of psychosis, but that cannabis use is "neither necessary nor sufficient" to cause psychosis.[68] A French review from 2009 came to a conclusion that cannabis use, particularly that before age 15, was a factor in the development of schizophrenic disorders.[69]
الآثار طويلة المدى المحتملة الأخرى
A 2008 National Institutes of Health study of 19 chronic heavy marijuana users with cardiac and cerebral abnormalities (averaging 28 g to 272 g (1 to 9+ oz) weekly) and 24 controls found elevated levels of apolipoprotein C-III (apoC-III) in the chronic smokers.[70] An increase in apoC-III levels induces the development of hypertriglyceridemia.
Pharmacology
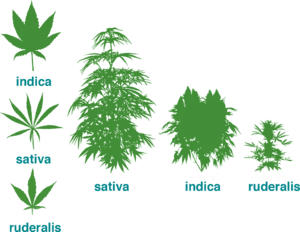
The genus Cannabis contains two species which produce useful amounts of psychoactive cannabinoids: Cannabis indica and Cannabis sativa, which are listed as Schedule I medicinal plants in the US;[4] a third species, Cannabis ruderalis, has few psychogenic properties.[4] Cannabis contains more than 460 compounds;[8] at least 80 of these are cannabinoids[71][72] – chemical compounds that interact with cannabinoid receptors in the brain.[4] As of 2012, more than 20 cannabinoids were being studied by the U.S. FDA.[73]
The most psychoactive cannabinoid found in the cannabis plant is tetrahydrocannabinol (or delta-9-tetrahydrocannabinol, commonly known as THC).[8] Other cannabinoids include delta-8-tetrahydrocannabinol, cannabidiol (CBD), cannabinol (CBN), cannabicyclol (CBL), cannabichromene (CBC) and cannabigerol (CBG); they have less psychotropic effects than THC, but may play a role in the overall effect of cannabis.[8] The most studied are THC, CBD and CBN.[61]
CB1 and CB2 are the primary cannabinoid receptors responsible for several of the effects of cannabinoids, although other receptors may play a role as well. Both belong to a group of receptors called G protein-coupled receptors (GPCRs). CB1 receptors are found in very high levels in the brain and are thought to be responsible for psychoactive effects.[74] CB2 receptors are found peripherally throughout the body and are thought to modulate pain and inflammation.[75]
Absorption
Cannabinoid absorption is dependent on its route of administration.
Inhaled and vaporized THC have similar absorption profiles to smoked THC, with a bioavailability ranging from 10 to 35%. Oral administration has the lowest bioavailability of approximately 6%, variable absorption depending on the vehicle used, and the longest time to peak plasma levels (2 to 6 hours) compared to smoked or vaporized THC.[76]
Similar to THC, CBD has poor oral bioavailability, approximately 6%. The low bioavailability is largely attributed to significant first-pass metabolism in the liver and erratic absorption from the gastrointestinal tract. However, oral administration of CBD has a faster time to peak concentrations (2 hours) than THC.[76]
Due to the poor bioavailability of oral preparations, alternative routes of administration have been studied, including sublingual and rectal. These alternative formulations maximize bioavailability and reduce first-pass metabolism. Sublingual administration in rabbits yielded bioavailability of 16% and time to peak concentration of 4 hours.[77] Rectal administration in monkeys doubled bioavailability to 13.5% and achieved peak blood concentrations within 1 to 8 hours after administration.[78]
Distribution
Like cannabinoid absorption, distribution is also dependent on route of administration. Smoking and inhalation of vaporized cannabis have better absorption than do other routes of administration, and therefore also have more predictable distribution.[78][79] THC is highly protein bound once absorbed, with only 3% found unbound in the plasma. It distributes rapidly to highly vascularized organs such as the heart, lungs, liver, spleen, and kidneys, as well as to various glands. Low levels can be detected in the brain, testes, and unborn fetuses, all of which are protected from systemic circulation via barriers.[80] THC further distributes into fatty tissues a few days after administration due to its high lipophilicity, and is found deposited in the spleen and fat after redistribution.[79][81][82]
Metabolism
Delta-9-THC is the primary molecule responsible for the effects of cannabis. Delta-9-THC is metabolized in the liver and turns into 11-OH-THC.[83] 11-OH-THC is the first metabolic product in this pathway. Both Delta-9-THC and 11-OH-THC are psychoactive. The metabolism of THC into 11-OH-THC plays a part in the heightened psychoactive effects of edible cannabis.[84]
Next, 11-OH-THC is metabolized in the liver into 11-COOH-THC, which is the second metabolic product of THC.[85] 11-COOH-THC is not psychoactive.[83]
Ingestion of edible cannabis products lead to a slower onset of effect than the inhalation of it because the THC travels to the liver first through the blood before it travels to the rest of the body. Inhaled cannabis can result in THC going directly to the brain, where it then travels from the brain back to the liver in recirculation for metabolism.[83] Eventually, both routes of metabolism result in the metabolism of psychoactive THC to inactive 11-COOH-THC.
Excretion
Due to substantial metabolism of THC and CBD, their metabolites are excreted mostly via feces, rather than by urine.[76][86] After delta-9-THC is hydroxylated into 11-OH-THC via CYP2C9, CYP2C19, and CYP3A4, it undergoes phase II metabolism into more than 30 metabolites, a majority of which are products of glucuronidation. Approximately 65% of THC is excreted in feces and 25% in the urine, while the remaining 10% is excreted by other means.[76] The terminal half-life of THC is 25 to 36 hours,[87] whereas for CBD it is 18 to 32 hours.[86]
CBD is hydroxylated by P450 liver enzymes into 7-OH-CBD. Its metabolites are products of primarily CYP2C19 and CYP3A4 activity, with potential activity of CYP1A1, CYP1A2, CYP2C9, and CYP2D6.[88] Similar to delta-9-THC, a majority of CBD is excreted in feces and some in the urine.[76] The terminal half-life is approximately 18–32 hours.[89]
التعاطي
Smoking has been the means of administration of cannabis for many users, but it is not suitable for the use of cannabis as a medicine.[90] It was the most common method of medical cannabis consumption in the US اعتبارا من 2013[تحديث].[4] It is difficult to predict the pharmacological response to cannabis because concentration of cannabinoids varies widely, as there are different ways of preparing it for consumption (smoked, applied as oils, eaten, infused into other foods, or drunk) and a lack of production controls.[4] The potential for adverse effects from smoke inhalation makes smoking a less viable option than oral preparations.[90] Cannabis vaporizers have gained popularity because of a perception among users that fewer harmful chemicals are ingested when components are inhaled via aerosol rather than smoke.[4] Cannabinoid medicines are available in pill form (dronabinol and nabilone) and liquid extracts formulated into an oromucosal spray (nabiximols).[4] Oral preparations are "problematic due to the uptake of cannabinoids into fatty tissue, from which they are released slowly, and the significant first-pass liver metabolism, which breaks down Δ9THC and contributes further to the variability of plasma concentrations".[90]
The US Food and Drug Administration (FDA) has not approved smoked cannabis for any condition or disease, as it deems that evidence is lacking concerning safety and efficacy.[91] The FDA issued a 2006 advisory against smoked medical cannabis stating: "marijuana has a high potential for abuse, has no currently accepted medical use in treatment in the United States, and has a lack of accepted safety for use under medical supervision."[91]
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
التاريخ
القديم
Cannabis, called má 麻 (meaning "hemp; cannabis; numbness") or dàmá 大麻 (with "big; great") in Chinese, was used in Taiwan for fiber starting about 10,000 years ago.[92] The botanist Hui-lin Li wrote that in China, "The use of Cannabis in medicine was probably a very early development. Since ancient humans used hemp seed as food, it was quite natural for them to also discover the medicinal properties of the plant."[93] Emperor Shen-Nung, who was also a pharmacologist, wrote a book on treatment methods in 2737 BCE that included the medical benefits of cannabis. He recommended the substance for many ailments, including constipation, gout, rheumatism, and absent-mindedness.[94] Cannabis is one of the 50 "fundamental" herbs in traditional Chinese medicine.[95]
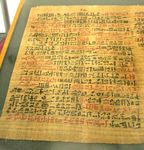
The Ebers Papyrus (c. 1550 BCE) from Ancient Egypt describes medical cannabis.[96] The ancient Egyptians used hemp (cannabis) in suppositories for relieving the pain of hemorrhoids.[97]
Surviving texts from ancient India confirm that cannabis' psychoactive properties were recognized, and doctors used it for treating a variety of illnesses and ailments, including insomnia, headaches, gastrointestinal disorders, and pain, including during childbirth.[98]
The Ancient Greeks used cannabis to dress wounds and sores on their horses,[99] and in humans, dried leaves of cannabis were used to treat nose bleeds, and cannabis seeds were used to expel tapeworms.[99]
In the medieval Islamic world, Arabic physicians made use of the diuretic, antiemetic, antiepileptic, anti-inflammatory, analgesic and antipyretic properties of Cannabis sativa, and used it extensively as medication from the 8th to 18th centuries.[100]
Landrace strains
Cannabis seeds may have been used for food, rituals or religious practices in ancient Europe and China.[101] Harvesting the plant led to the spread of cannabis throughout Eurasia about 10,000 to 5,000 years ago, with further distribution to the Middle East and Africa about 2,000 to 500 years ago.[101] A landrace strain of cannabis developed over centuries.[102] They are cultivars of the plant that originated in one specific region.
Widely cultivated strains of cannabis, such as "Afghani" or "Hindu Kush", are indigenous to the Pakistan and Afghanistan regions, while "Durban Poison" is native to Africa.[101] There are approximately 16 landrace strains of cannabis identified from Pakistan, Jamaica, Africa, Mexico, Central America and Asia.[103]
الحديث
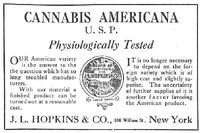
An Irish physician, William Brooke O'Shaughnessy, is credited with introducing cannabis to Western medicine.[104] O'Shaughnessy discovered cannabis in the 1830s while living abroad in India, where he conducted numerous experiments investigating the drug's medical utility (noting in particular its analgesic and anticonvulsant effects).[105] He returned to England with a supply of cannabis in 1842, after which its use spread through Europe and the United States.[106] Cannabis was entered into the United States Pharmacopeia in 1850.[105]
The use of cannabis in medicine began to decline by the end of the 19th century, due to difficulty in controlling dosages and the rise in popularity of synthetic and opium-derived drugs.[106] Also, the advent of the hypodermic syringe allowed these drugs to be injected for immediate effect, in contrast to cannabis which is not water-soluble and therefore cannot be injected.[106]
In the United States, the medical use of cannabis further declined with the passage of the Marihuana Tax Act of 1937, which imposed new regulations and fees on physicians prescribing cannabis.[107] Cannabis was removed from the U.S. Pharmacopeia in 1941, and officially banned for any use with the passage of the Controlled Substances Act of 1970.[106]
Cannabis began to attract renewed interest as medicine in the 1970s and 1980s, in particular due to its use by cancer and AIDS patients who reported relief from the effects of chemotherapy and wasting syndrome.[108] In 1996, California became the first U.S. state to legalize medical cannabis in defiance of federal law.[109] In 2001, Canada became the first country to adopt a system regulating the medical use of cannabis.[110]
The Ebers Papyrus (c. 1550 BCE) from Ancient Egypt has a prescription for medical marijuana applied directly for inflammation.
"قنب طبي" باللغة المصرية القديمة، بالكتابة الديموطية. من بردية برلين رقم 3038، الصفحة السابعة، السطر الثامن، الوصفة رقم 81، استخدام القنب الطبي كخافض للحرارة والالتهاب.
المجتمع والثقافة
الوضع القانوني
See also countries that have decriminalized or where enforcement is limited.
Countries that have legalized the medical use of cannabis include Australia,[111] Brazil,[112] Canada,[113] Chile,[113] Colombia,[113] Croatia,[114] Cyprus,[115] Czech Republic,[113] Finland,[116] Germany,[117] Greece,[118] Israel,[119] Italy,[120] Jamaica,[121] Lebanon,[122] Luxembourg,[123] North Macedonia,[124] Malta,[125] the Netherlands,[113] New Zealand,[126] Peru,[127] Poland,[128] Portugal,[129] Sri Lanka,[130] Thailand,[131] the United Kingdom,[132] and Uruguay.[113] Other countries have more restrictive laws that allow only the use of isolated cannabinoid drugs such as Sativex or Epidiolex.[133][134] Countries with the most relaxed policies include Canada,[135] Uruguay,[113] and the Netherlands,[113] where cannabis can be purchased without need for a prescription. In Mexico, THC content of medical cannabis is limited to one percent.[136] The same limit applies in Switzerland, but no prescription is required to purchase.[137] In the United States, the legality of medical cannabis varies by state.[12]
Cannabis is in Schedule IV of the United Nations' Single Convention on Narcotic Drugs, making it subject to special restrictions. Article 2 provides for the following, in reference to Schedule IV drugs:
A Party shall, if in its opinion the prevailing conditions in its country render it the most appropriate means of protecting the public health and welfare, prohibit the production, manufacture, export and import of, trade in, possession or use of any such drug except for amounts which may be necessary for medical and scientific research only, including clinical trials therewith to be conducted under or subject to the direct supervision and control of the Party.[138]
The convention thus allows countries to outlaw cannabis for all non-research purposes but lets nations choose to allow use for medical and scientific purposes if they believe total prohibition is not the most appropriate means of protecting health and welfare. The convention requires that states that permit the production or use of medical cannabis must operate a licensing system for all cultivators, manufacturers, and distributors and ensure that the total cannabis market of the state shall not exceed that required "for medical and scientific purposes".[138]
الولايات المتحدة
In the United States, the use of cannabis for medical purposes is legal in 33 states, four out of five permanently inhabited U.S. territories, and the District of Columbia.[12] An additional 14 states have more restrictive laws allowing the use of low-THC products.[12] Cannabis remains illegal at the federal level under the Controlled Substances Act, which classifies it as a Schedule I drug with a high potential for abuse and no accepted medical use. In December 2014, however, the Rohrabacher–Farr amendment, which prohibits the Justice Department from prosecuting individuals acting in accordance with state medical cannabis laws, was signed into federal law.[139]
الاقتصاديات
التوزيع
The method of obtaining medical cannabis varies by region and by legislation. In the US, most consumers grow their own or buy it from cannabis dispensaries in states where it is legal.[4][140] Marijuana vending machines for selling or dispensing cannabis are in use in the United States and are planned to be used in Canada.[141] In 2014, the startup Meadow began offering on-demand delivery of medical marijuana in the San Francisco Bay Area, through their mobile app.[142]
التأمين
In the United States, health insurance companies may not pay for a medical marijuana prescription as the Food and Drug Administration must approve any substance for medicinal purposes. Before this can happen, the FDA must first permit the study of the medical benefits and drawbacks of the substance, which it has not done since it was placed on Schedule I of the Controlled Substances Act in 1970. Therefore, all expenses incurred fulfilling a medical marijuana prescription will possibly be incurred as out-of-pocket.[143] However, the New Mexico Court of Appeals has ruled that workers' compensation insurance must pay for prescribed marijuana as part of the state's Medical Cannabis Program.[144]
مواقف المنظمات الطبية
Medical organizations that have issued statements in support of allowing access to medical cannabis include the American Nurses Association,[9] American Public Health Association,[145] American Medical Student Association,[146] National Multiple Sclerosis Society,[147] Epilepsy Foundation,[148] and Leukemia & Lymphoma Society.[149]
Organizations that have issued statements in opposition to the legalization of medical cannabis include the American Academy of Pediatrics,[11] American Psychiatric Association,[150] and American Society of Addiction Medicine.[151] However, the AAP also supports rescheduling for the purpose of facilitating research.[11]
The American Medical Association[152] and American College of Physicians[153] do not take a position on the legalization of medical cannabis, but have called for the Schedule I classification of cannabis to be reviewed. The American Academy of Family Physicians similarly does not take a position, but does support rescheduling in order to facilitate research.[10] The American Cancer Society[154] and American Psychological Association[155] have noted the obstacles that exist for conducting research on cannabis, and have called on the federal government to better enable scientific study of the drug.
Cancer Research UK say that while cannabis is being studied for therapeutic potential, "claims that there is solid 'proof' that cannabis or cannabinoids can cure cancer is highly misleading to patients and their families, and builds a false picture of the state of progress in this area".[156]
الاستخدام الترفيهي
The authors of a report on a 2011 survey of medical cannabis users say that critics have suggested that some users "game the system" to obtain medical cannabis ostensibly for treatment of a condition, but then use it for nonmedical purposes – though the truth of this claim is hard to measure.[157] The report authors suggested rather that medical cannabis users occupied a "continuum" between medical and nonmedical use.[157]
أسماء تجارية
In the US, the FDA has approved two oral cannabinoids for use as medicine: dronabinol and nabilone.[4] Dronabinol, synthetic THC, is listed as Schedule II.[158] Nabilone, a synthetic cannabinoid, is also Schedule II, indicating high potential for side effects and addiction.[73] Both received approval for sale in the US in 1985, under the brand names Marinol and Cesamet.[159] Nabiximols, an oromucosal spray derived from two strains of Cannabis sativa and containing THC and CBD,[73] is not approved in the United States, but is approved in several European countries, Canada, and New Zealand as of 2013.[4] As of 2018, medical marijuana in Canada is being legally distributed to registered patients in bud, drops and capsule forms by such companies as Canopy Growth Corp. and Aurora Cannabis.
| Generic medication |
Brand name(s) |
Country | Licensed indications |
|---|---|---|---|
| Nabilone | Cesamet | U.S., Canada | Antiemetic (treatment of nausea or vomiting) associated with chemotherapy that has failed to respond adequately to conventional therapy[4] |
| Dronabinol | Marinol | ||
| Syndros | U.S. | Anorexia associated with AIDS–related weight loss[4] | |
| Nabiximols | Sativex | Canada, New Zealand, majority of the EU[160] |
Limited treatment for spasticity and neuropathic pain associated with multiple sclerosis and intractable cancer pain.[4] |
As an antiemetic, these medications are usually used when conventional treatment for nausea and vomiting associated with cancer chemotherapy fail to work.[4]
Nabiximols is used for treatment of spasticity associated with MS when other therapies have not worked, and when an initial trial demonstrates "meaningful improvement".[4] Trials for FDA approval in the US are underway.[4] It is also approved in several European countries for overactive bladder and vomiting.[73] When sold under the trade name Sativex as a mouth spray, the prescribed daily dose in Sweden delivers a maximum of 32.4 mg of THC and 30 mg of CBD; mild to moderate dizziness is common during the first few weeks.[161]
Relative to inhaled consumption, peak concentration of oral THC is delayed, and it may be difficult to determine optimal dosage because of variability in patient absorption.[4]
In 1964, Albert Lockhart and Manley West began studying the health effects of traditional cannabis use in Jamaican communities. They developed, and in 1987 gained permission to market, the pharmaceutical "Canasol", one of the first cannabis extracts.[162]
أبحاث
Medical cannabis research includes any medical research on using cannabis as a treatment for any medical condition. For reasons including increased popular support of cannabis use, a trend of cannabis legalization, and the perception of medical usefulness, more scientists are doing medical cannabis research. Medical cannabis is unusually broad as a treatment for many conditions, each of which has its own state of research. Similarly, various countries conduct and respond to medical cannabis research in different ways.
انظر أيضاً
المراجع
- ^ Murnion B (ديسمبر 2015). "Medicinal cannabis". Australian Prescriber. 38 (6): 212–5. doi:10.18773/austprescr.2015.072. PMC 4674028. PMID 26843715.
- ^ "What is medical marijuana?". National Institute of Drug Abuse. يوليو 2015. Retrieved 19 أبريل 2016.
The term medical marijuana refers to using the whole unprocessed marijuana plant or its basic extracts to treat a disease or symptom.
- ^ "Release the strains". Nature Medicine. 21 (9): 963. سبتمبر 2015. doi:10.1038/nm.3946. PMID 26340110.
- ^ أ ب ت ث ج ح خ د ذ ر ز س ش ص ض ط ظ ع غ ف ق ك ل م Borgelt LM, Franson KL, Nussbaum AM, Wang GS (فبراير 2013). "The pharmacologic and clinical effects of medical cannabis" (PDF). Pharmacotherapy. 33 (2): 195–209. doi:10.1002/phar.1187. PMID 23386598.
- ^ أ ب ت ث ج ح خ Whiting PF, Wolff RF, Deshpande S, Di Nisio M, Duffy S, Hernandez AV, Keurentjes JC, Lang S, Misso K, Ryder S, Schmidlkofer S, Westwood M, Kleijnen J (23 يونيو 2015). "Cannabinoids for Medical Use: A Systematic Review and Meta-analysis". JAMA. 313 (24): 2456–73. doi:10.1001/jama.2015.6358. PMID 26103030.
- ^ Jensen B, Chen J, Furnish T, Wallace M (أكتوبر 2015). "Medical Marijuana and Chronic Pain: a Review of Basic Science and Clinical Evidence". Current Pain and Headache Reports. 19 (10): 50. doi:10.1007/s11916-015-0524-x. PMID 26325482.
- ^ أ ب Commissioner, Office of the (10 يونيو 2019). "FDA and Marijuana". FDA (in الإنجليزية).
- ^ أ ب ت ث Ben Amar M (أبريل 2006). "Cannabinoids in medicine: A review of their therapeutic potential". Journal of Ethnopharmacology (Review). 105 (1–2): 1–25. CiteSeerX 10.1.1.180.308. doi:10.1016/j.jep.2006.02.001. PMID 16540272.
- ^ أ ب Therapeutic Use of Marijuana and Related Cannabinoids, American Nurses Association, 2016, https://www.nursingworld.org/~4ad4a8/globalassets/docs/ana/therapeutic-use-of-marijuana-and-related-cannabinoids.pdf
- ^ أ ب "AAFP Releases Marijuana, Cannabinoids Position Paper". American Academy of Family Physicians. 20 سبتمبر 2019. Retrieved 6 أكتوبر 2019.
- ^ أ ب ت American Academy of Pediatrics Reaffirms Opposition to Legalizing Marijuana for Recreational or Medical Use, American Academy of Pediatrics, 26 January 2015, https://www.aap.org/en-us/about-the-aap/aap-press-room/Pages/American-Academy-of-Pediatrics-Reaffirms-Opposition-to-Legalizing-Marijuana-for-Recreational-or-Medical-Use.aspx, retrieved on 30 July 2017
- ^ أ ب ت ث "State Medical Marijuana Laws". National Conference of State Legislatures. 27 يونيو 2018. Retrieved 3 يوليو 2018.
- ^ "Marijuana as Medicine". National Institute on Drug Abuse. يوليو 2019.
- ^ أ ب ت Consumer Reports (28 أبريل 2016). "Up in Smoke: Does Medical Marijuana Work?". Consumer Reports. Retrieved 24 مايو 2016.
- ^ أ ب Schubart CD, Sommer IE, Fusar-Poli P, de Witte L, Kahn RS, Boks MP (يناير 2014). "Cannabidiol as a potential treatment for psychosis" (PDF). European Neuropsychopharmacology. 24 (1): 51–64. doi:10.1016/j.euroneuro.2013.11.002. PMID 24309088.
- ^ أ ب ت Koppel BS, Brust JC, Fife T, Bronstein J, Youssof S, Gronseth G, Gloss D (أبريل 2014). "Systematic review: efficacy and safety of medical marijuana in selected neurologic disorders: report of the Guideline Development Subcommittee of the American Academy of Neurology". Neurology. 82 (17): 1556–63. doi:10.1212/WNL.0000000000000363. PMC 4011465. PMID 24778283.
- ^ أ ب Sachs J, McGlade E, Yurgelun-Todd D (أكتوبر 2015). "Safety and Toxicology of Cannabinoids". Neurotherapeutics. 12 (4): 735–46. doi:10.1007/s13311-015-0380-8. PMC 4604177. PMID 26269228.
- ^ قالب:Cite website
- ^ Gilson, Aaron M.; LeBaron, Virginia T.; Vyas, Marianne Beare (1 يناير 2018). "The use of cannabis in response to the opioid crisis: A review of the literature". Nursing Outlook. 66 (1): 56–65. doi:10.1016/j.outlook.2017.08.012. ISSN 0029-6554. PMID 28993073.
- ^ American College of Obstetricians Gynecologists Committee on Obstetric Practice (يوليو 2015). "Committee Opinion No. 637: Marijuana Use During Pregnancy and Lactation". Obstetrics and Gynecology. 126 (1): 234–8. doi:10.1097/01.AOG.0000467192.89321.a6. PMID 26241291.
- ^ أ ب Grotenhermen F, Müller-Vahl K (يوليو 2012). "The therapeutic potential of cannabis and cannabinoids". Deutsches Arzteblatt International. 109 (29–30): 495–501. doi:10.3238/arztebl.2012.0495. PMC 3442177. PMID 23008748.
- ^ Bowles DW, O'Bryant CL, Camidge DR, Jimeno A (يوليو 2012). "The intersection between cannabis and cancer in the United States". Critical Reviews in Oncology/Hematology (Review). 83 (1): 1–10. doi:10.1016/j.critrevonc.2011.09.008. PMID 22019199.
- ^ أ ب Wang T, Collet JP, Shapiro S, Ware MA (يونيو 2008). "Adverse effects of medical cannabinoids: a systematic review". CMAJ (Review). 178 (13): 1669–78. doi:10.1503/cmaj.071178. PMC 2413308. PMID 18559804.
- ^ Jordan K, Sippel C, Schmoll HJ (سبتمبر 2007). "Guidelines for antiemetic treatment of chemotherapy-induced nausea and vomiting: past, present, and future recommendations". The Oncologist (Review). 12 (9): 1143–50. doi:10.1634/theoncologist.12-9-1143. PMID 17914084.
- ^ Nicolson SE, Denysenko L, Mulcare JL, Vito JP, Chabon B (مايو–يونيو 2012). "Cannabinoid hyperemesis syndrome: a case series and review of previous reports". Psychosomatics (Review, case series). 53 (3): 212–9. doi:10.1016/j.psym.2012.01.003. PMID 22480624.
- ^ Phillips RS, Friend AJ, Gibson F, Houghton E, Gopaul S, Craig JV, Pizer B (فبراير 2016). "Antiemetic medication for prevention and treatment of chemotherapy-induced nausea and vomiting in childhood" (PDF). The Cochrane Database of Systematic Reviews. 2: CD007786. doi:10.1002/14651858.CD007786.pub3. PMID 26836199.
- ^ Lutge EE, Gray A, Siegfried N (أبريل 2013). "The medical use of cannabis for reducing morbidity and mortality in patients with HIV/AIDS". The Cochrane Database of Systematic Reviews (Review). 4 (4): CD005175. doi:10.1002/14651858.CD005175.pub3. PMID 23633327.
- ^ أ ب Aviram J, Samuelly-Leichtag G (سبتمبر 2017). "Efficacy of Cannabis-Based Medicines for Pain Management: A Systematic Review and Meta-Analysis of Randomized Controlled Trials". Pain Physician. 20 (6): E755–E796. PMID 28934780.
- ^ Nugent SM, Morasco BJ, O'Neil ME, Freeman M, Low A, Kondo K, Elven C, Zakher B, Motu'apuaka M, Paynter R, Kansagara D (سبتمبر 2017). "The Effects of Cannabis Among Adults With Chronic Pain and an Overview of General Harms: A Systematic Review". Annals of Internal Medicine. 167 (5): 319–331. doi:10.7326/M17-0155. PMID 28806817.
- ^ Kahan M, Srivastava A, Spithoff S, Bromley L (ديسمبر 2014). "Prescribing smoked cannabis for chronic noncancer pain: preliminary recommendations". Canadian Family Physician. 60 (12): 1083–90. PMC 4264803. PMID 25500598.
- ^ Andreae MH, Carter GM, Shaparin N, Suslov K, Ellis RJ, Ware MA, Abrams DI, Prasad H, Wilsey B, Indyk D, Johnson M, Sacks HS (ديسمبر 2015). "Inhaled Cannabis for Chronic Neuropathic Pain: A Meta-analysis of Individual Patient Data". The Journal of Pain. 16 (12): 1221–1232. doi:10.1016/j.jpain.2015.07.009. PMC 4666747. PMID 26362106.
- ^ Deshpande A, Mailis-Gagnon A, Zoheiry N, Lakha SF (أغسطس 2015). "Efficacy and adverse effects of medical marijuana for chronic noncancer pain: Systematic review of randomized controlled trials". Canadian Family Physician. 61 (8): e372–81. PMC 4541447. PMID 26505059.
- ^ Lynch ME, Campbell F (نوفمبر 2011). "Cannabinoids for treatment of chronic non-cancer pain; a systematic review of randomized trials". British Journal of Clinical Pharmacology (Review). 72 (5): 735–44. doi:10.1111/j.1365-2125.2011.03970.x. PMC 3243008. PMID 21426373.
- ^ Carter GT, Flanagan AM, Earleywine M, Abrams DI, Aggarwal SK, Grinspoon L (أغسطس 2011). "Cannabis in palliative medicine: improving care and reducing opioid-related morbidity". The American Journal of Hospice & Palliative Care (Review). 28 (5): 297–303. doi:10.1177/1049909111402318. PMID 21444324.
- ^ Lakhan SE, Rowland M (ديسمبر 2009). "Whole plant cannabis extracts in the treatment of spasticity in multiple sclerosis: a systematic review". BMC Neurology (Review). 9: 59. doi:10.1186/1471-2377-9-59. PMC 2793241. PMID 19961570.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Clark PA, Capuzzi K, Fick C (ديسمبر 2011). "Medical marijuana: medical necessity versus political agenda". Medical Science Monitor (Review). 17 (12): RA249–61. doi:10.12659/MSM.882116. PMC 3628147. PMID 22129912.
- ^ Oreja-Guevara C (أكتوبر 2012). "[Treatment of spasticity in multiple sclerosis: new perspectives regarding the use of cannabinoids]". Revista de Neurología (Review) (in الإسبانية). 55 (7): 421–30. PMID 23011861.
- ^ Black N, Stockings E, Campbell G, Tran LT, Zagic D, Hall WD, Farrell M, Degenhardt L (ديسمبر 2019). "Cannabinoids for the treatment of mental disorders and symptoms of mental disorders: a systematic review and meta-analysis". Lancet Psychiatry (Systematic review & meta-analysis). 6 (12): 995–1010. doi:10.1016/S2215-0366(19)30401-8. PMC 6949116. PMID 31672337.
- ^ أ ب Washington, Tabitha A.; Brown, Khalilah M.; Fanciullo, Gilbert J. (2012). "Chapter 31: Medical Cannabis". Pain. Oxford University Press. p. 165. ISBN 978-0-19-994274-9.
Proponents of medical cannabis site its safety, but there studies in later years that support that smoking of marijuana is associated with risk for dependence and that THC alters the structures of cells in the brain
{{cite book}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Gage SH, Hickman M, Zammit S (أبريل 2016). "Association Between Cannabis and Psychosis: Epidemiologic Evidence". Biological Psychiatry. 79 (7): 549–56. doi:10.1016/j.biopsych.2015.08.001. hdl:1983/b8fb2d3b-5a55-4d07-97c0-1650b0ffc05d. PMID 26386480.
- ^ Barceloux, Donald G (2012). "Chapter 60: Marijuana (Cannabis sativa L.) and synthetic cannabinoids". Medical Toxicology of Drug Abuse: Synthesized Chemicals and Psychoactive Plants. pp. 886–931. ISBN 978-0-471-72760-6.
- ^ أ ب ت Hall W, Solowij N (نوفمبر 1998). "Adverse effects of cannabis". Lancet. 352 (9140): 1611–6. doi:10.1016/S0140-6736(98)05021-1. PMID 9843121.
- ^ "Sativex Oral Mucosal Spray Public Assessment Report. Decentralized Procedure" (PDF). United Kingdom Medicines and Healthcare Products Regulatory Agency. p. 93. Retrieved 7 مايو 2015.
There is clear evidence that recreational cannabis can produce a transient toxic psychosis in larger doses or in susceptible individuals, which is said to characteristically resolve within a week or so of absence (Johns 2001). Transient psychotic episodes as a component of acute intoxication are well-documented (Hall et al 1994)
- ^ D'Souza DC, Sewell RA, Ranganathan M (أكتوبر 2009). "Cannabis and psychosis/schizophrenia: human studies". European Archives of Psychiatry and Clinical Neuroscience. 259 (7): 413–31. doi:10.1007/s00406-009-0024-2. PMC 2864503. PMID 19609589.
- ^ "Drug Abuse Warning Network, 2011. National Estimates of Drug-Related Emergency Department Visits" (PDF). U.S. Department of Health and Human Services. 2011. Retrieved 8 مايو 2015.
- ^ "www.samhsa.gov".
- ^ أ ب ت Volkow ND, Baler RD, Compton WM, Weiss SR (يونيو 2014). "Adverse health effects of marijuana use". The New England Journal of Medicine. 370 (23): 2219–27. doi:10.1056/NEJMra1402309. PMC 4827335. PMID 24897085.
- ^ Hall W (يناير 2015). "What has research over the past two decades revealed about the adverse health effects of recreational cannabis use?" (PDF). Addiction. 110 (1): 19–35. doi:10.1111/add.12703. PMID 25287883.
- ^ Zehra, Amna; Burns, Jamie; Liu, Christopher Kure; Manza, Peter; Wiers, Corinde E.; Volkow, Nora D.; Wang, Gene-Jack (2018). "Cannabis Addiction and the Brain: a Review". Journal of Neuroimmune Pharmacology. 13 (4): 438–452. doi:10.1007/s11481-018-9782-9. ISSN 1557-1890. PMC 6223748. PMID 29556883.
- ^ Maisto, Stephen; Galizio, Mark; Connors, Gerard (2014). Drug Use and Abuse. Cengage Learning. p. 278. ISBN 978-1-305-17759-8.
{{cite book}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ أ ب Tashkin DP (يونيو 2013). "Effects of marijuana smoking on the lung". Annals of the American Thoracic Society. 10 (3): 239–47. doi:10.1513/annalsats.201212-127fr. PMID 23802821.
- ^ Hashibe M, Straif K, Tashkin DP, Morgenstern H, Greenland S, Zhang ZF (أبريل 2005). "Epidemiologic review of marijuana use and cancer risk". Alcohol. 35 (3): 265–75. doi:10.1016/j.alcohol.2005.04.008. PMID 16054989.
- ^ "Does smoking cannabis cause cancer?". Cancer Research UK. 20 سبتمبر 2010. Archived from the original on 29 يوليو 2012. Retrieved 9 يناير 2013.
{{cite journal}}: Cite journal requires|journal=(help) - ^ Tashkin, Donald (مارس 1997). "Effects of marijuana on the lung and its immune defenses". UCLA School of Medicine. Retrieved 23 يونيو 2012.
{{cite journal}}: Cite journal requires|journal=(help) - ^ A. Riecher-Rössler (2014). Comorbidity of Mental and Physical Disorders. Karger Medical and Scientific Publishers. p. 88. ISBN 978-3-318-02604-7.
- ^ Cottencin O, Karila L, Lambert M, Arveiller C, Benyamina A, Boissonas A, Goudemand M, Reynaud M (ديسمبر 2010). "Cannabis arteritis: review of the literature". Journal of Addiction Medicine. 4 (4): 191–6. doi:10.1097/ADM.0b013e3181beb022. PMID 21769037.
- ^ Thomas G, Kloner RA, Rezkalla S (يناير 2014). "Adverse cardiovascular, cerebrovascular, and peripheral vascular effects of marijuana inhalation: what cardiologists need to know". The American Journal of Cardiology. 113 (1): 187–90. doi:10.1016/j.amjcard.2013.09.042. PMID 24176069.
- ^ Jones RT (نوفمبر 2002). "Cardiovascular system effects of marijuana". Journal of Clinical Pharmacology (Review). 42 (S1): 58S–63S. doi:10.1002/j.1552-4604.2002.tb06004.x. PMID 12412837.
- ^ "Withdrawal Symptoms From Smoking Pot?". WebMD.
- ^ Hall W, Degenhardt L (أكتوبر 2009). "Adverse health effects of non-medical cannabis use". Lancet. 374 (9698): 1383–91. doi:10.1016/s0140-6736(09)61037-0. PMID 19837255.
- ^ أ ب Gordon AJ, Conley JW, Gordon JM (ديسمبر 2013). "Medical consequences of marijuana use: a review of current literature". Current Psychiatry Reports (Review). 15 (12): 419. doi:10.1007/s11920-013-0419-7. PMID 24234874.
- ^ "Get Medical Marijuana Card Online in 10 Mins - Medical Marijuana Doctor". Get a Medical Marijuana Card Online - California Cannabis Doctors (in الإنجليزية الأمريكية). Retrieved 5 أكتوبر 2019.
- ^ Crean RD, Crane NA, Mason BJ (مارس 2011). "An evidence based review of acute and long-term effects of cannabis use on executive cognitive functions". Journal of Addiction Medicine. 5 (1): 1–8. doi:10.1097/ADM.0b013e31820c23fa. PMC 3037578. PMID 21321675.
- ^ Martín-Santos R, Fagundo AB, Crippa JA, Atakan Z, Bhattacharyya S, Allen P, Fusar-Poli P, Borgwardt S, Seal M, Busatto GF, McGuire P (مارس 2010). "Neuroimaging in cannabis use: a systematic review of the literature" (PDF). Psychological Medicine. 40 (3): 383–98. doi:10.1017/S0033291709990729. PMID 19627647.
- ^ Grant I, Gonzalez R, Carey CL, Natarajan L, Wolfson T (يوليو 2003). "Non-acute (residual) neurocognitive effects of cannabis use: a meta-analytic study". Journal of the International Neuropsychological Society. 9 (5): 679–89. doi:10.1017/S1355617703950016. PMID 12901774.
{{cite journal}}: Unknown parameter|lay-url=ignored (help); Unknown parameter|laydate=ignored (help); Unknown parameter|laysource=ignored (help) - ^ Large M, Sharma S, Compton MT, Slade T, Nielssen O (يونيو 2011). "Cannabis use and earlier onset of psychosis: a systematic meta-analysis". Archives of General Psychiatry. 68 (6): 555–61. doi:10.1001/archgenpsychiatry.2011.5. PMID 21300939.
- ^ Semple DM, McIntosh AM, Lawrie SM (مارس 2005). "Cannabis as a risk factor for psychosis: systematic review". Journal of Psychopharmacology. 19 (2): 187–94. doi:10.1177/0269881105049040. PMID 15871146.
- ^ Arseneault L, Cannon M, Witton J, Murray RM (فبراير 2004). "Causal association between cannabis and psychosis: examination of the evidence". The British Journal of Psychiatry. 184 (2): 110–7. doi:10.1192/bjp.184.2.110. PMID 14754822.
- ^ Laqueille X (سبتمبر 2009). "[Is cannabis a vulnerability factor in schizophrenic disorders]" [Is cannabis is a vulnerability factor of schizophrenic disorders?]. Archives de Pediatrie. 16 (9): 1302–5. doi:10.1016/j.arcped.2009.03.016. PMID 19640690.
- ^ Jayanthi S, Buie S, Moore S, Herning RI, Better W, Wilson NM, Contoreggi C, Cadet JL (يناير 2010). "Heavy marijuana users show increased serum apolipoprotein C-III levels: evidence from proteomic analyses". Molecular Psychiatry. 15 (1): 101–12. doi:10.1038/mp.2008.50. PMC 2797551. PMID 18475272.
{{cite journal}}: Unknown parameter|lay-url=ignored (help); Unknown parameter|laydate=ignored (help); Unknown parameter|laysource=ignored (help) - ^ Downer EJ, Campbell VA (يناير 2010). "Phytocannabinoids, CNS cells and development: a dead issue?". Drug and Alcohol Review (Review). 29 (1): 91–8. doi:10.1111/j.1465-3362.2009.00102.x. PMID 20078688.
- ^ Burns TL, Ineck JR (فبراير 2006). "Cannabinoid analgesia as a potential new therapeutic option in the treatment of chronic pain". The Annals of Pharmacotherapy (Review). 40 (2): 251–60. doi:10.1345/aph.1G217. PMID 16449552.
- ^ أ ب ت ث Svrakic DM, Lustman PJ, Mallya A, Lynn TA, Finney R, Svrakic NM (2012). "Legalization, decriminalization & medicinal use of cannabis: a scientific and public health perspective". Missouri Medicine (Review). 109 (2): 90–8. PMC 6181739. PMID 22675784.
- ^ Mackie K (مايو 2008). "Cannabinoid receptors: where they are and what they do". Journal of Neuroendocrinology. 20 Suppl 1: 10–4. doi:10.1111/j.1365-2826.2008.01671.x. PMID 18426493.
- ^ Whiteside GT, Lee GP, Valenzano KJ (2007). "The role of the cannabinoid CB2 receptor in pain transmission and therapeutic potential of small molecule CB2 receptor agonists". Current Medicinal Chemistry. 14 (8): 917–36. doi:10.2174/092986707780363023. PMID 17430144.
- ^ أ ب ت ث ج Gaston TE, Friedman D (مايو 2017). "Pharmacology of cannabinoids in the treatment of epilepsy". Epilepsy & Behavior. Cannabinoids and Epilepsy. 70 (Pt B): 313–318. doi:10.1016/j.yebeh.2016.11.016. PMID 28087250.
- ^ Mannila J, Järvinen T, Järvinen K, Tervonen J, Jarho P (مارس 2006). "Sublingual administration of Delta9-tetrahydrocannabinol/beta-cyclodextrin complex increases the bioavailability of Delta9-tetrahydrocannabinol in rabbits". Life Sciences. 78 (17): 1911–4. doi:10.1016/j.lfs.2005.08.025. PMID 16266727.
- ^ أ ب Huestis MA (أغسطس 2007). "Human cannabinoid pharmacokinetics". Chemistry & Biodiversity. 4 (8): 1770–804. doi:10.1002/cbdv.200790152. PMC 2689518. PMID 17712819.
- ^ أ ب Badowski ME (سبتمبر 2017). "A review of oral cannabinoids and medical marijuana for the treatment of chemotherapy-induced nausea and vomiting: a focus on pharmacokinetic variability and pharmacodynamics". Cancer Chemotherapy and Pharmacology. 80 (3): 441–449. doi:10.1007/s00280-017-3387-5. PMC 5573753. PMID 28780725.
- ^ Nahas GG (أبريل 2001). "The pharmacokinetics of THC in fat and brain: resulting functional responses to marihuana smoking". Human Psychopharmacology. 16 (3): 247–255. doi:10.1002/hup.258. PMID 12404577.
- ^ Bridgeman MB, Abazia DT (مارس 2017). "Medicinal Cannabis: History, Pharmacology, And Implications for the Acute Care Setting". P & T. 42 (3): 180–188. PMC 5312634. PMID 28250701.
- ^ Nahas, Gabriel G.; Sutin, Kenneth M.; Harvey, David J.; Agurell, Stig (5 أبريل 1999). Marihuana and Medicine. Springer Science & Business Media. ISBN 978-1-59259-710-9.
{{cite book}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ أ ب ت "Human Metabolism of THC". Sapiensoup Blog (in الإنجليزية الأمريكية). 21 ديسمبر 2016. Retrieved 1 نوفمبر 2017.
- ^ "11-Hydroxy-THC - Increased Potency That Explains the Effect of Edibles? - Prof of Pot". profofpot.com (in الإنجليزية الأمريكية). Retrieved 1 نوفمبر 2017.
- ^ "Toxicology Litigation Support: Marijuana". consultox.com. Retrieved 1 نوفمبر 2017.
- ^ أ ب Devinsky O, Cilio MR, Cross H, Fernandez-Ruiz J, French J, Hill C, Katz R, Di Marzo V, Jutras-Aswad D, Notcutt WG, Martinez-Orgado J, Robson PJ, Rohrback BG, Thiele E, Whalley B, Friedman D (يونيو 2014). "Cannabidiol: pharmacology and potential therapeutic role in epilepsy and other neuropsychiatric disorders". Epilepsia. 55 (6): 791–802. doi:10.1111/epi.12631. PMC 4707667. PMID 24854329.
- ^ Grotenhermen F (1 أبريل 2003). "Pharmacokinetics and pharmacodynamics of cannabinoids". Clinical Pharmacokinetics. 42 (4): 327–60. doi:10.2165/00003088-200342040-00003. PMID 12648025.
- ^ Juřica, Ondřej Zendulka, Gabriela Dovrtělová, Kristýna Nosková, Miroslav Turjap, Alexandra Šulcová, Lumír Hanuš and Jan (29 فبراير 2016). "Cannabinoids and Cytochrome P450 Interactions". Current Drug Metabolism (in الإنجليزية). 17 (3).
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Ohlsson A, Lindgren JE, Andersson S, Agurell S, Gillespie H, Hollister LE (فبراير 1986). "Single-dose kinetics of deuterium-labelled cannabidiol in man after smoking and intravenous administration". Biomedical & Environmental Mass Spectrometry. 13 (2): 77–83. doi:10.1002/bms.1200130206. PMID 2937482.
- ^ أ ب ت Curtis A, Clarke CE, Rickards HE (أكتوبر 2009). "Cannabinoids for Tourette's Syndrome". The Cochrane Database of Systematic Reviews (Review) (4): CD006565. doi:10.1002/14651858.CD006565.pub2. PMID 19821373.
- ^ أ ب "Inter-agency advisory regarding claims that smoked marijuana is a medicine" (Press release). fda.gov. 20 أبريل 2006. Retrieved 24 ديسمبر 2012.
- ^ Abel, Ernest L. (1980). "Cannabis in the Ancient World". Marihuana: the first twelve thousand years. New York City: Plenum Publishers. ISBN 978-0-306-40496-2.
{{cite book}}: External link in|chapterurl=|chapterurl=ignored (|chapter-url=suggested) (help)[صفحة مطلوبة] - ^ Li, Hui-Lin (1974). "An Archaeological and Historical Account of Cannabis in China", Economic Botany 28.4:437–448, p. 444.
- ^ Bloomquist, Edward (1971). Marijuana: The Second Trip. California: Glencoe Press.
- ^ Wong, Ming (1976). La Médecine chinoise par les plantes. Paris: Tchou. OCLC 2646789.[صفحة مطلوبة]
- ^ "The Ebers Papyrus The Oldest (confirmed) Written Prescriptions For Medical Marihuana era 1,550 BC". onlinepot.org. Retrieved 10 يونيو 2008.
- ^ Pain, Stephanie (15 ديسمبر 2007). "The Pharaoh's pharmacists". New Scientist. Reed Business Information Ltd.
- ^ Touw M (1981). "The religious and medicinal uses of Cannabis in China, India and Tibet". Journal of Psychoactive Drugs. 13 (1): 23–34. doi:10.1080/02791072.1981.10471447. PMID 7024492.
- ^ أ ب Butrica, James L. (2002). "The Medical Use of Cannabis Among the Greeks and Romans" (PDF). Journal of Cannabis Therapeutics. 2 (2): 51–70. doi:10.1300/J175v02n02_04. Retrieved 8 نوفمبر 2014.
- ^ Lozano, Indalecio (2001). "The Therapeutic Use of Cannabis sativa (L.) in Arabic Medicine". Journal of Cannabis Therapeutics. 1: 63–70. CiteSeerX 10.1.1.550.1717. doi:10.1300/J175v01n01_05.
- ^ أ ب ت Holland, Julie (Editor) (2010). The Pot Book: A Complete Guide to Cannabis. New York: Simon and Schuster. ISBN 978-1594778988. Retrieved 22 أبريل 2018.
{{cite book}}:|author=has generic name (help) - ^ Evert, Ray F.; Eichhorn, Susan E. (2013). Raven Biology of Plants (8th ed.). New York, NY: W. H. Freeman and Company. pp. 213–217. ISBN 978-1-4292-1961-7.
{{cite book}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Evert, Ray F.; Eichhorn, Susan E. (2013). Raven Biology of Plants (8th ed.). New York, NY: W.H. Freeman and Company. pp. 501–504. ISBN 9781429219617.
{{cite book}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Alison Mack; Janet Joy (7 ديسمبر 2000). Marijuana As Medicine?: The Science Beyond the Controversy. National Academies Press. pp. 15–. ISBN 978-0-309-06531-3.
- ^ أ ب Booth, Martin (يونيو 2005). Cannabis: A History. New York: St. Martin's Press. ISBN 978-0-312-42494-7.
- ^ أ ب ت ث Grinspoon, Lester; Bakalar, James (1997). Marihuana, the Forbidden Medicine (Revised and expanded ed.). Yale University Press. ISBN 978-0-300-07086-6.
{{cite book}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Pacula, Rosalie Piccardo (فبراير 2002). "State Medical Marijuana Laws: Understanding the Laws and Their Limitations" (PDF). Journal of Public Health Policy. 23 (4): 413–439. CiteSeerX 10.1.1.202.2274. doi:10.2307/3343240. JSTOR 3343240.
- ^ Joy, Janet E.; Watson, Stanley J.; Benson, John A. (1999). "Marijuana and Medicine -- Assessing the Science Base" (PDF). Washington, D.C.: National Academy Press. Archived from the original (PDF) on 23 يناير 2018. Retrieved 28 يوليو 2017.
{{cite news}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ "History of Marijuana as Medicine – 2900 BC to Present". ProCon.org. Retrieved 27 يوليو 2017.
- ^ "Marijuana's journey to legal health treatment: the Canadian experience". CBC News. 17 أغسطس 2009. Retrieved 27 يوليو 2017.
- ^ Jolly, William (28 فبراير 2018). "Medicinal Marijuana Legal In Australia". Canstar. Retrieved 16 يوليو 2018.
- ^ Ponieman, Natan (3 ديسمبر 2019). "Brazil Regulates Sale Of Medical Marijuana Products". Benzinga. Retrieved 10 ديسمبر 2019.
- ^ أ ب ت ث ج ح خ د Williams, Sean (15 مايو 2016). "10 Countries (Aside From the U.S.) Where Some Form of Medical Marijuana Is Legal". The Motley Fool. Retrieved 5 نوفمبر 2017.
- ^ Veselica, Lajla (15 أكتوبر 2015). "Croatia legalises marijuana for medical use". Yahoo News. AFP. Retrieved 4 نوفمبر 2017.
- ^ "Cyprus begins to distribute medical cannabis". InCyprus. 22 مايو 2017. Archived from the original on 9 يونيو 2017. Retrieved 11 نوفمبر 2017.
- ^ "Legal status of cannabis in Finland – An overview". Sensi Seeds. Retrieved 4 نوفمبر 2017.
- ^ Senthilingam, Meera (6 مارس 2017). "Germany joins the global experiment on marijuana legalization". CNN.com. Retrieved 4 نوفمبر 2017.
- ^ Revesz, Rachael (3 يوليو 2017). "Greece legalises marijuana for medical purposes". The Independent. Retrieved 4 نوفمبر 2017.
- ^ Schwartz, Yardena (24 أغسطس 2017). "How the Booming Israeli Weed Industry Is Changing American Pot". Rollingstone.com. Retrieved 4 نوفمبر 2017.
- ^ Samuels, Gabriel (26 يوليو 2016). "Italian army aims to produce 'the best-quality' medical marijuana after finding current batches deficient". The Independent. Retrieved 4 نوفمبر 2017.
- ^ Bud, Monterey (19 مارس 2018). "Jamaica's Kaya Farms Becomes First Medical Marijuana Dispensary To Open". marijuana.com. Retrieved 16 يوليو 2018.
- ^ "Lebanon Legalizes Cannabis Farming for Medicinal Use". The New York Times. Reuters. 21 أبريل 2020.
- ^ Pritchard, Heledd (29 يونيو 2018). "Cannabis for medical use legalised in Luxembourg". Luxembourg Times. Retrieved 8 يوليو 2018.
- ^ Marusic, Sinisa Jakov (1 يونيو 2016). "Macedonia Allows Medical Marijuana in Pharmacies". Balkan Insight. Retrieved 4 نوفمبر 2017.
- ^ Pace, Maria (27 مارس 2018). "Malta has officially legalised medical cannabis". Malta Today. Retrieved 24 أغسطس 2018.
- ^ Ainge Roy, Eleanor (11 ديسمبر 2018). "New Zealand passes laws to make medical marijuana widely available". The Guardian. Retrieved 20 يناير 2019.
- ^ Collyns, Dan (20 أكتوبر 2017). "Peru legalises medical marijuana in move spurred by mother's home lab". The Guardian. Retrieved 4 نوفمبر 2017.
- ^ "Medical use of cannabis officially legal in Poland". Radio Poland. PAP. 11 فبراير 2017. Retrieved 4 نوفمبر 2017.
- ^ Lamers, Matt (21 يونيو 2018). "Portugal passes medical cannabis law, opens domestic market". Marijuana Business Daily. Retrieved 24 أغسطس 2018.
- ^ South Asia Regional Profile, United Nations Office on Drugs and Crime, 15 September 2005, https://www.unodc.org/pdf/india/publications/south_Asia_Regional_Profile_Sept_2005/13_srilanka.pdf, retrieved on 2 February 2019
- ^ Mosbergen, Dominique (25 ديسمبر 2018). "Thailand Approves Medical Marijuana In Regional First". HuffPost. Retrieved 20 يناير 2019.
- ^ "Medicinal cannabis products to be legalised". BBC. 26 يوليو 2018. Retrieved 28 يوليو 2018.
- ^ "Sativex (delta-9-tetrahydrocannabinol and cannabidiol)". GW Pharmaceuticals. Archived from the original on 10 ديسمبر 2017. Retrieved 5 نوفمبر 2017.
- ^ Medical use of cannabis and cannabinoids, European Monitoring Centre for Drugs and Drug Addiction, December 2018, http://www.emcdda.europa.eu/system/files/publications/10171/20185584_TD0618186ENN_PDF.pdf
- ^ Sapra, Bani (20 يونيو 2018). "Canada becomes second nation in the world to legalize marijuana". CNN. Retrieved 3 يوليو 2018.
- ^ Janikian, Michelle (14 سبتمبر 2017). "Legal Pot In Mexico: Everything You Need to Know". Rolling Stone. Retrieved 5 نوفمبر 2017.
- ^ Depetris, Marina; Miller, John (21 مارس 2017). "Swiss cannabis entrepreneurs develop craving for low-potency pot". Reuters. Retrieved 5 نوفمبر 2017.
{{cite news}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ أ ب "Single Convention on Narcotic Drugs, 1961 As amended by the 1972 Protocol" (PDF). International Narcotics Control Board. United Nations. 13 مارس 1961. pp. 2–3. Retrieved 17 أغسطس 2009.
- ^ Ingraham, Christopher (13 يونيو 2017). "Jeff Sessions personally asked Congress to let him prosecute medical-marijuana providers". The Washington Post. Retrieved 9 يوليو 2017.
- ^ Timothy B. Wheeler (11 أكتوبر 2014). "Medical marijuana fees stir debate in Maryland". The Baltimore Sun. Retrieved 12 أكتوبر 2014.
- ^ Blackwell, Tom (16 أكتوبر 2013). "The pot vending machine's first foreign market? Canada, of course, 'a seed for the rest of the world'". National Post. Retrieved 4 ديسمبر 2013.
- ^ "Uber-For-Weed Startup Meadow Lights Up In San Francisco". TechCrunch. AOL. 14 أكتوبر 2014. Retrieved 22 يناير 2016.
- ^ Clark, Tonya Body (10 فبراير 2015). "The Medical Marijuana Debate". Compliance Corner. Wolters Kluwer Financial Services. Retrieved 26 فبراير 2015.
- ^ Peters, Joey (29 يونيو 2015). "Court: Employer can't block workers' comp for medical marijuana". NM Political Report. Retrieved 30 يونيو 2015.
- ^ "Resolution on Medical Marijuana". druglibrary.org. Retrieved 30 يوليو 2017.
- ^ "House of Delegates 2017, Resolution: A8" (PDF). amsa.org. American Medical Student Association. Retrieved 30 يوليو 2017.
- ^ "Medical Marijuana (Cannabis) FAQs". National Multiple Sclerosis Society. Retrieved 30 يوليو 2017.
- ^ Gattone, Philip M.; Lammert, Warreb (20 فبراير 2014). "Epilepsy Foundation Calls for Increased Medical Marijuana Access and Research" (Press release). Washington, D.C.: Epilepsy Foundation. Retrieved 30 يوليو 2017.
{{cite press release}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ "Medical Marijuana Use and Research" (PDF). maps.org. Leukemia & Lymphoma Society. Retrieved 30 يوليو 2017.
- ^ "Position Statement on Marijuana as Medicine" (PDF). American Psychiatric Association. Retrieved 30 يوليو 2017.
- ^ "Public Policy Statement on Marijuana, Cannabinoids and Legalization" (PDF). American Society of Addiction Medicine. 21 سبتمبر 2015.
- ^ Use of Cannabis for Medicinal Purposes, American Medical Association, 2009, https://www.ama-assn.org/sites/default/files/media-browser/public/about-ama/councils/Council%20Reports/council-on-science-public-health/i09-csaph-medical-marijuana.pdf
- ^ Supporting Research into the Therapeutic Role of Marijuana, American College of Physicians, February 2016, https://www.acponline.org/acp_policy/policies/supporting_research_therapeutic_role_of_marijuana_2016.pdf
- ^ "Marijuana and Cancer". American Cancer Society. Retrieved 12 يوليو 2017.
- ^ "Marijuana research: Overcoming the barriers". American Psychological Association. 14 سبتمبر 2017. Retrieved 9 أكتوبر 2017.
- ^ Arney, Kat (25 يوليو 2012). "Cannabis, cannabinoids and cancer – the evidence so far". Cancer Research UK. Archived from the original on 11 فبراير 2014.
- ^ أ ب Reinarman C, Nunberg H, Lanthier F, Heddleston T (2011). "Who are medical marijuana patients? Population characteristics from nine California assessment clinics". Journal of Psychoactive Drugs (Review). 43 (2): 128–35. doi:10.1080/02791072.2011.587700. PMID 21858958.
- ^ "Final Rule: Placement of FDA-Approved Products of Oral Solutions Containing Dronabinol [(-)-delta-9-trans-tetrahydrocannabinol (delta-9-THC)] in Schedule II". U.S. Department of Justice. Retrieved 2 فبراير 2018.
- ^ Clark, Amy (16 مايو 2006). "'New' Pot Pill For Chemo Patients". CBS News. Associated Press. Retrieved 26 يوليو 2017.
- ^ Abuhasira R, Shbiro L, Landschaft Y (مارس 2018). "Medical use of cannabis and cannabinoids containing products - Regulations in Europe and North America". European Journal of Internal Medicine. 49: 2–6. doi:10.1016/j.ejim.2018.01.001. PMID 29329891.
- ^ "Produkt – FASS Allmänhet". fass.se.
- ^ Dr Farid F. Youssef. "Cannabis Unmasked: What it is and why it does what it does". UWIToday: June 2010. http://sta.uwi.edu/uwitoday/archive/june_2010/article9.asp
للاستزادة
- National Academies Of Sciences, Engineering; Health Medicine, Division; Board on Population Health Public Health Practice; Committee on the Health Effects of Marijuana: An Evidence Review Research Agenda (2017). The Health Effects of Cannabis and Cannabinoids: The Current State of Evidence and Recommendations for Research. National Academies of Sciences, Engineering, and Medicine: The National Academies Press. doi:10.17226/24625. ISBN 978-0-309-45304-2. PMID 28182367.
{{cite book}}:|website=ignored (help)
وصلات خارجية
- القنب الطبي at Curlie, links to websites about medical cannabis
- Information on Cannabis and Cannabinoids from the U.S. National Cancer Institute
- Information on cannabis (marihuana, marijuana) and the cannabinoids from Health Canada
- The Center for Medicinal Cannabis Research of the University of California
- Medical Marijuana – a 2014–2015 three-part CNN documentary produced by Sanjay Gupta
- CS1 maint: unflagged free DOI
- CS1 الإسبانية-language sources (es)
- CS1 errors: unsupported parameter
- CS1 الإنجليزية الأمريكية-language sources (en-us)
- مقالات بالمعرفة بحاجة لذكر رقم الصفحة بالمصدر from August 2010
- مقالات ينقصها مصادر موثوقة
- مقالات ينقصها مصادر موثوقة from December 2013
- CS1 errors: generic name
- صفحات بالمعرفة فيها قوالب حماية خاطئة
- صفحات شبه محمية للأبد في المعرفة
- Use dmy dates from October 2017
- Use American English from October 2017
- All Wikipedia articles written in American English
- Short description matches Wikidata
- Articles with specifically marked weasel-worded phrases from April 2017
- Articles with hatnote templates targeting a nonexistent page
- جميع المقالات التي فيها عبارات متقادمة
- CS1 errors: periodical ignored
- Articles with Curlie links
- Medicinal use of cannabis
- مضادات القيء
- مضادات أكسدة
- Biologically-based therapies
- عطارة
- أخلاقيات الطب
- نباتات طبية
- سياسات دوائية
- عقاقير